Summary: PTEN deficiency drives an increased expression of LOX. LOX attracts macrophages which protect glioblastoma brain cancer cells and provide growth factor support for the tumor, a new mouse study reveals.
Source: MD Anderson Cancer Center
A common genetic deficiency empowers glioblastoma to broadcast a molecular message to the wrong type of immune cell, summoning macrophages that protect and nurture the brain tumor instead of attacking it, researchers at The University of Texas MD Anderson Cancer Center report in Cancer Cell.
The team’s work in mouse models of glioblastoma that lack functional cancer-suppressor gene PTEN points to new potential targets for treating the most common and lethal brain tumor, said senior author Ronald DePinho, M.D., professor of Cancer Biology and past president of MD Anderson.
About a third of all glioblastomas are PTEN-deficient. Median survival for glioblastoma is about 12 to 15 months, and only 5 percent of patients survive for five years.
“We’ve identified a symbiotic circuit that is activated in PTEN-deficient glioblastoma which creates a mutually supportive relationship between the cancer cell and macrophages that come into the tumor microenvironment and provide growth factor support for the tumor,” DePinho said.
Macrophages engulf and digest microbes, cellular debris and tumor cells as part of an immune response, and they secrete cytokines that affect other cells. They are bipolar. In their M1 form, they actively assist immune response and inhibit tumor growth. In M2, they are in repair mode, helping post-immune recovery, which can also promote cancer growth and progression.
Up to half the live cells found in glioblastoma are macrophages. They are major components forming the tumor microenvironment, the researchers note.
First author Peiwen Chen, Ph.D., postdoctoral fellow in Cancer Biology, DePinho and colleagues set out to find common mutations in glioblastoma associated with immune changes in the tumor microenvironment.
They not only defined the pathway that brings macrophages into glioblastoma but also pinpointed a growth factor secreted by the macrophages that in turn protects cancer cells from programmed cell death and fuels the growth of new blood vessels.
“We first found that only PTEN-deficiency, but not other common genetic alterations, is associated with macrophage infiltration in glioblastoma,” Chen said.
In a series of experiments, in PTEN knockout cell lines and later in mouse models of glioblastoma, they showed:
- With PTEN down, a gene called YAP1 is activated, a transcription factor that increases expression of LOX, a novel potent attractor of macrophages;
- LOX connects to the β1 integrin-PYK2 pathway on macrophages, spurring their migration into the tumor microenvironment;
- Macrophages directly aid glioma cells by secreting the growth factor SPP1, which the team showed increases cancer cell survival and blood vessel formation to protect the tumors.
Thwarting LOX shrinks tumors, blocks macrophage infiltration
The team developed human xenograft mouse models of glioblastoma that had high expression of LOX, YAP1, and macrophage markers. Depleting LOX in these models using either shRNA, the small-molecule LOX inhibitor BAPN or an anti-LOX antibody impaired tumor growth and significantly reduced macrophage infiltration.
LOX inhibition in four PTEN-deficient glioblastoma mouse models extended survival in all models.
Blocking LOX had no impact on glioma cell proliferation but did increase cancer cell programmed cell death and decrease the formation of tumor-supporting blood vessels.
As a first check on the possible impact of their findings on humans, the team performed unsupervised clustering of an established macrophage signature in 489 human glioblastoma samples from The Cancer Genome Atlas.
By clustering cases by macrophage-high (201), macrophage-medium (153) and macrophage-low (135) groups, as well as analyzing tumor-associated macrophages compared to blood-derived monocytes from glioblastoma mouse models and patients, they identified eight genes correlated with macrophage infiltration in patients. Among the eight, SPP1 was the gene with the greatest increase in expression.
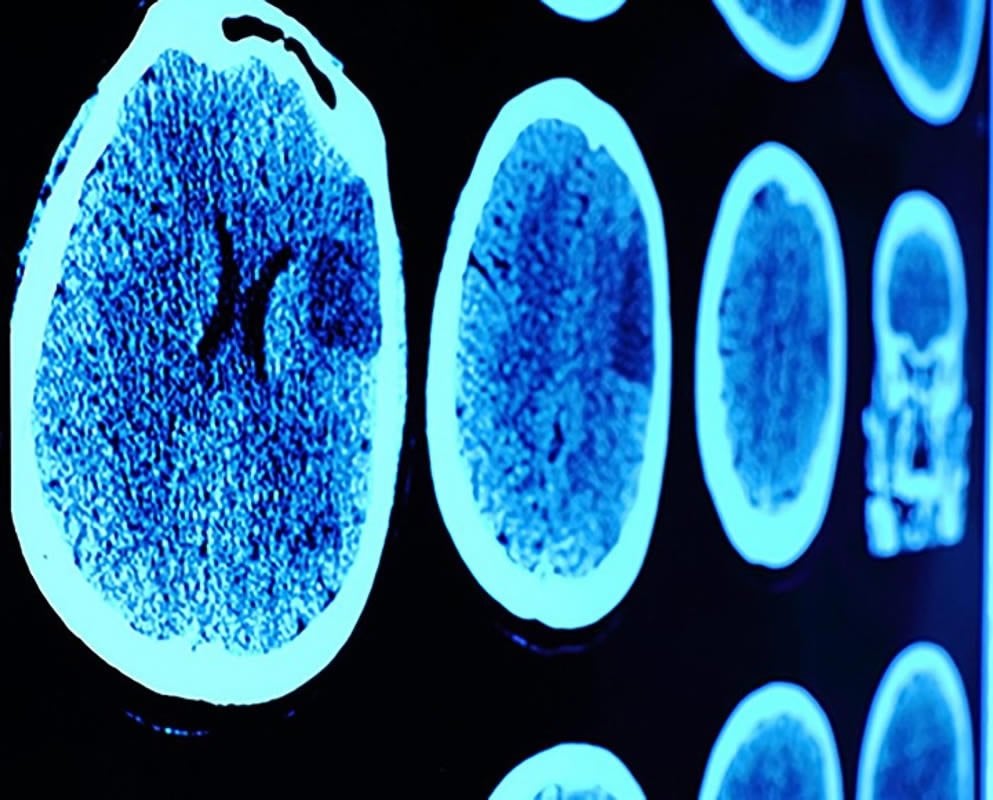
The macrophage-high group had more frequent PTEN mutations or deletions, higher YAP1 and LOX expression and poorer survival than patients in the macrophage-low cluster.
LOX, SPP1 are new targets for PTEN-deficient glioblastoma
The most targetable components in the pathway are LOX and SPP1, DePinho said, with drugs under development to hit both genes.
“The results in mice are compelling enough and the correlative studies in human glioblastoma provide additional confidence to motivate the testing of this approach in a clinical setting of recurrent glioblastoma patients,” DePinho said.
It would be important to enlist only those with PTEN-deficient tumors, he said, because their research shows LOX inhibition does not work in tumors with wild-type PTEN.
Co-authors with Chen and DePinho are Di Zhao, Ph.D., Xin Liang, M.D., Jiexi Li, Andrew Chang, M.D., Zhengdao Lan, M.D., Ph.D., Denise Spring, Ph.D., and Alan Wang, Ph.D., of Cancer Biology; Jun Li, Ph.D., of Genomic Medicine; and Verlene Henry and Ganesh Rao, M.D., of Neurosurgery. Jiexi Li is a graduate student in the MD Anderson/UTHealth Graduate School of Biomedical Sciences.
DePinho holds the Harry Graves Burkhart III Distinguished University Chair in Cancer Biology.
Funding: This research was supported by the Cancer Research Institute Irvington Postdoctoral Fellowship, the Caroline Ross Endowed Fellowship, The Harold C. and Mary L. Daily Endowment Fellowship, the Burkhart III Distinguished University Chair in Cancer Research Endowment, Clayton & Modesta Williams Cancer Research Fund, the Emerson Collective Award, and grants from the National Cancer Institute of the National Institutes of Health, (P01 CA117969 14, R01 CA084628, R01 CA231349, K99 CA226360, R01 NS094615) including MD Anderson’s Cancer Center Support Grant from the NCI (P30CA16672).
Source:
MD Anderson Cancer Center
Media Contacts:
Scott Merville – MD Anderson Cancer Center
Image Source:
The image is adapted from the MD Anderson Cancer Center news release.
Original Research: Closed access
“Symbiotic Macrophage-Glioma Cell Interactions Reveal Synthetic Lethality in PTEN-Null Glioma”. Ronald DePinho et al.
Cancer Cell. doi:10.1016/j.ccell.2019.05.003
Abstract
Symbiotic Macrophage-Glioma Cell Interactions Reveal Synthetic Lethality in PTEN-Null Glioma
Highlights
• PTEN deficiency in GBM drives macrophage infiltration via upregulation of LOX
• LOX is directly regulated by YAP1 in PTEN-deficient GBM
• LOX recruits macrophages into GBM via the β1 integrin-PYK2 pathway
• LOX inhibition impairs PTEN-deficient GBM progression by decreasing TAM-derived SPP1
Summary
Heterotypic interactions across diverse cell types can enable tumor progression and hold the potential to expand therapeutic interventions. Here, combined profiling and functional studies of glioma cells in glioblastoma multiforme (GBM) models establish that PTEN deficiency activates YAP1, which directly upregulates lysyl oxidase (LOX) expression. Mechanistically, secreted LOX functions as a potent macrophage chemoattractant via activation of the β1 integrin-PYK2 pathway in macrophages. These infiltrating macrophages secrete SPP1, which sustains glioma cell survival and stimulates angiogenesis. In PTEN-null GBM models, LOX inhibition markedly suppresses macrophage infiltration and tumor progression. Correspondingly, YAP1-LOX and β1 integrin-SPP1 signaling correlates positively with higher macrophage density and lower overall survival in GBM patients. This symbiotic glioma-macrophage interplay provides therapeutic targets specifically for PTEN-deficient GBM.