In addition to treating depression, a commonly used antidepressant medication also protects against compounds that can cause memory loss and dementia, a Loyola University Medical Center study has found.
The study found that blood levels of two neurotoxic compounds dropped significantly in depressed patients after they were treated with the antidepressant escitalopram (Lexapro®).
The study, published in the Journal of Psychiatric Research, provides new insights into how the immune system responds to depression.
Stress and depression interact in a vicious cycle. Stress can lead to depression in susceptible individuals. In turn, depression, if not treated, causes stress. This stimulates the body’s immune system to fight stress and depression, as it would a disease or infection. Revving up the immune system, which includes the inflammatory response, initially protects against stress. But over time, chronic inflammation can cause a range of health problems.
In this vicious cycle, depression can trigger an inflammatory response, which in turn can exacerbate depression, said Angelos Halaris, MD, PhD, lead author of the study and a professor in the Department of Psychiatry and Behavioral Neurosciences of Loyola University Chicago Stritch School of Medicine.
“It behooves us to diagnose depression early, treat it vigorously to achieve remission and work to prevent its relapse,” Dr. Halaris said.
The study compared 30 severely depressed patients with 27 healthy subjects. The patients were treated with escitalopram and followed for 12 weeks. Some patients dropped out of the study due to side effects of escitalopram or other reasons. Of the 20 patients who completed the entire study, 80 percent reported complete or partial relief from their depression.
To examine the inflammatory response, researchers measured blood levels of nine substances secreted by the immune system. At the beginning of the study, average levels of all nine of these substances were higher in the depressed patients than in the healthy subjects. The differences were statistically significant with four of these substances (hsCRP, TNFα, IL6 and MCP1).
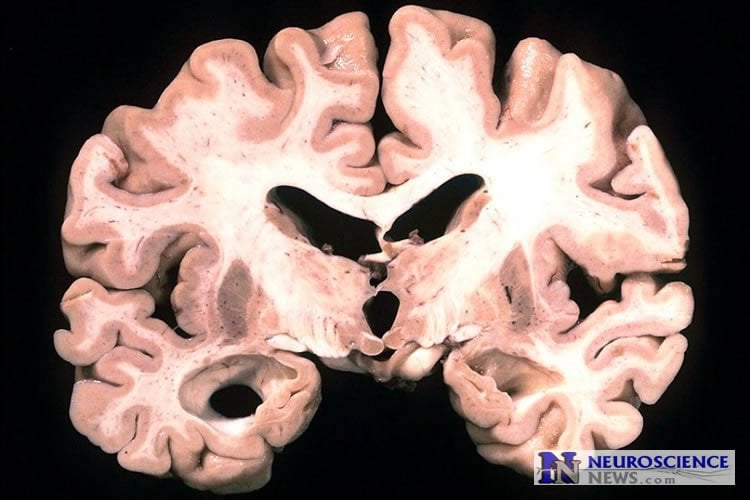
The inflammatory response can lead to the production of neurotoxic compounds that can kill brain cells, leading to memory loss and dementia if the depression goes untreated or fails to respond adequately to treatment. The study found that among patients treated with escitalopram, levels of two neurotoxic compounds dropped significantly. Levels of 3-hydroxykynurenine fell by more than two-thirds between week 8 and week 12. Levels of quinolinic acid dropped 50 percent during the first eight weeks and were lower at the end of the study than at the beginning.
Escitalopram belongs to a class of antidepressants called selective serotonin reuptake inhibitors (SSRIs). It’s possible that other SSRIs, such as Prozac®, Paxil® and Zoloft®, also could protect against neurotoxins, but this would have to be confirmed with other studies, Dr. Halaris said.
The study is limited by the small number of subjects. But it should stimulate interest in replicating the findings with larger groups over a longer period of time, researchers wrote.
The study is titled “Does escitalopram reduce neurotoxity in major depression?”
In addition to Dr. Halaris, other co-authors are Vidushi Savant, MD, Edwin Meresh, MD, Debra Hoppensteadt, PhD, Jawed Fareed, PhD, and James Sinacore, PhD, of Loyola; Aye-Mu Myint, MD, PhD of the University of Munich; and Edwin Lim, PhD, and Gilles Guillemin, PhD, of the Australian School of Advanced Medicine.
Source: Jim Ritter – Loyola University Health System
Image Source: The image is in the public domain
Original Research: Abstract for “Does escitalopram reduce neurotoxicity in major depression?” by Angelos Halaris, Aye-Mu Myint, Vidushi Savant, Edwin Meresh, Edwin Lim, Gilles Guillemin, Debra Hoppensteadt, Jawed Fareed, and James Sinacore in Journal of Psychiatric Research. Published online August 2015 doi:10.1016/j.jpsychires.2015.04.026
Abstract
Does escitalopram reduce neurotoxicity in major depression?
A pro-inflammatory state and a dysregulation in the tryptophan/kynurenine pathway have been documented in depression. This study examined whether treatment with the SSRI, escitalopram (ESC), could suppress inflammation and favorably shift metabolites of the kynurenine pathway in patients with major depressive disorder (MDD) within the utilized treatment period. Twenty seven healthy control subjects were included for comparison. Thirty patients were enrolled after completing baseline assessments. They received a 12-week ESC monotherapy. Twenty subjects were completers. Clinical assessments were carried out at each visit using the HAM-D, HAM-A, CGI and BDI rating scales. Blood samples were collected at each assessment and stored until analyzed. Cytokines were analyzed with Randox multiplex assay and tryptophan and kynurenine metabolites were analyzed using HPLC/GCMS. Baseline plasma concentrations of hsCRP, TNFα, IL6 and MCP-1 were significantly higher in patients compared to healthy controls. IL10 trended toward an increase. Baseline plasma IL1β correlated significantly with IL1α, and IL4. Patients showed significant improvement in all outcome measures with a high remission rate. Significant correlations were obtained between specific symptoms and certain biomarkers at baseline but these correlations must be viewed as very preliminary. During ESC treatment concentrations of inflammatory biomarkers did not change except for TNFα that trended lower. Metabolites and ratios of the tryptophan/kynurenine pathway showed reductions of the neurotoxic metabolites, 3-hydroxykynurenine and quinolinic acid, 3-hydroxykynurenine/kynurenine, quinolinic acid/tryptophan, kynurenic acid/quinolinic acid and quinolinic acid/3-hydroxykynurenine. The results indicate that ESC may exert its antidepressant effect in part through inhibition of synthesis of certain neurotoxic kynurenine metabolites and possibly also through reduction of the inflammatory response, although there was no concordance in the time course of changes between antidepressant efficacy and reversal of the pro-inflammatory status.
“Does escitalopram reduce neurotoxicity in major depression?” by Angelos Halaris, Aye-Mu Myint, Vidushi Savant, Edwin Meresh, Edwin Lim, Gilles Guillemin, Debra Hoppensteadt, Jawed Fareed, and James Sinacore in Journal of Psychiatric Research. Published online August 2015 doi:10.1016/j.jpsychires.2015.04.026







