Summary: Researchers have discovered how the body is able to initiate repair mechanisms which can limit the extent of damage to the myelin sheath. The findings could help with the development of new therapies for multiple sclerosis.
Source: Charite.
Diseases such as multiple sclerosis are characterized by damage to the ‘myelin sheath’, a protective covering wrapped around nerve cells akin to insulation around an electrical wire. Researchers from Charité – Universitätsmedizin Berlin have discovered how the body initiates repair mechanisms which will limit the extent of any damage to this sheath. Their findings, which provide a basis for the development of new drugs to treat multiple sclerosis, have been published in the eminent journal Nature Communications.
Multiple sclerosis is the most common autoimmune disease of the central nervous system. Estimates suggest that more than 200,000 people are affected by the disease in Germany alone. People with multiple sclerosis experience vision and sensory problems, as well as impaired coordination or even paralysis. These symptoms are caused by the disruption of nerve impulses in either the brain or the spinal cord. This disruption occurs when the body’s immune system attacks the myelin sheath, which is wrapped around the body’s nerve fibers and provides electrical insulation. When the myelin sheath is no longer intact, communication between nerve cells is impaired. Researchers across the globe are searching for new ways to repair the myelin sheath and, in doing so, are looking to reduce neurological symptoms in people with multiple sclerosis. Researchers from Charité have now moved a decisive step closer to this goal.
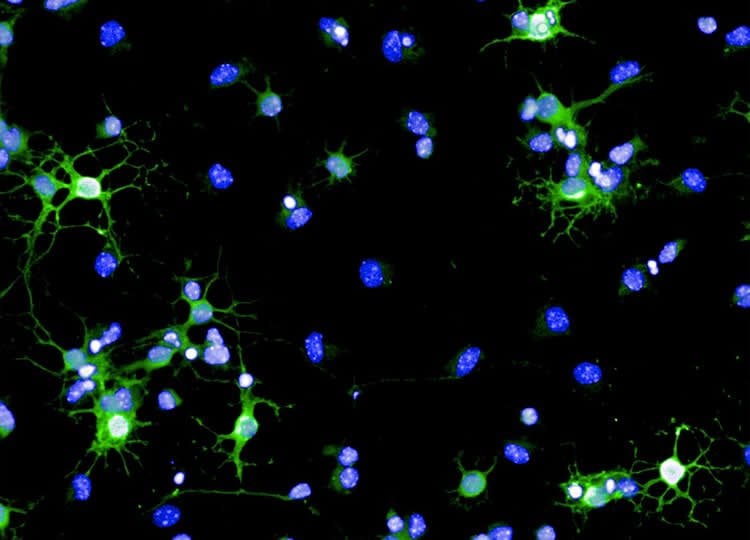
Charité’s research team decided to take a closer look at the body’s innate ability to heal itself, knowing that, under certain conditions, the central nervous system is capable of repairing damage to the myelin sheath. Specific molecular signals enable stem cells to differentiate into myelin repair cells (oligodendrocytes), which reside in a small stem-cell niche in the brain. Once they leave this niche, these repair cells migrate to where myelin damage has occurred in order to restore the affected nerve cells’ electrical insulation. Until now, very little had been known about the molecular signals responsible for initiating this myelin regeneration mechanism. “We have found that the Chi3l3 protein plays a central role in the body’s capacity to produce new myelin-forming oligodendrocytes,” says the study’s first author, Dr. Sarah-Christin Staroßom of Charité’s Institute for Medical Immunology. A researcher at the NeuroCure Cluster of Excellence and the Experimental and Clinical Research Center (ECRC), Dr. Staroßom explains the protein’s role as follows: “The Chi3l3 protein initiates the differentiation of neural stem cells into myelin repair cells, which restore the electrical insulation around damaged nerve cells.”
Using a mouse model, the research team were able to show that a reduction in Chi3l3 levels in the brain significantly impairs the body’s capacity for oligodendrocyte production, while a Chi3l3 infusion leads to an increase in the production of myelin repair cells. The same reaction was observed during an in vitro experiment using human cells. “We hope to use this knowledge to develop a new generation of drugs that can be used in the treatment of multiple sclerosis,” explains Dr. Staroßom. “As a next step, we will study in greater detail whether Chi3l3 or related proteins can be used to reduce the neurological symptoms of patients with multiple sclerosis.”
Funding: German Research Council, Oppenheim research Prize, National Institutes of Health funded this study.
Source: Sarah-Christin Staroßom – Charite
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is credited to Staroßom/Charité.
Original Research: Open access research for “Chi3l3 induces oligodendrogenesis in an experimental model of autoimmune neuroinflammation” by Sarah C. Starossom, Juliana Campo Garcia, Tim Woelfle, Silvina Romero-Suarez, Marta Olah, Fumihiro Watanabe, Li Cao, Ada Yeste, John J. Tukker, Francisco J. Quintana, Jaime Imitola, Franziska Witzel, Dietmar Schmitz, Markus Morkel, Friedemann Paul, Carmen Infante-Duarte & Samia J. Khoury in Nature Communications. Published January 15 2019.
doi:10.1038/s41467-018-08140-7
[cbtabs][cbtab title=”MLA”]Charite”Helping Cells to Help Themselves May Benefit Multiple Sclerosis.” NeuroscienceNews. NeuroscienceNews, 22 January 2019.
<https://neurosciencenews.com/multiple-sclerosis-cell-help-10613/>.[/cbtab][cbtab title=”APA”]Charite(2019, January 22). Helping Cells to Help Themselves May Benefit Multiple Sclerosis. NeuroscienceNews. Retrieved January 22, 2019 from https://neurosciencenews.com/multiple-sclerosis-cell-help-10613/[/cbtab][cbtab title=”Chicago”]Charite”Helping Cells to Help Themselves May Benefit Multiple Sclerosis.” https://neurosciencenews.com/multiple-sclerosis-cell-help-10613/ (accessed January 22, 2019).[/cbtab][/cbtabs]
Abstract
Chi3l3 induces oligodendrogenesis in an experimental model of autoimmune neuroinflammation
In demyelinating diseases including multiple sclerosis (MS), neural stem cells (NSCs) can replace damaged oligodendrocytes if the local microenvironment supports the required differentiation process. Although chitinase-like proteins (CLPs) form part of this microenvironment, their function in this differentiation process is unknown. Here, we demonstrate that murine Chitinase 3-like-3 (Chi3l3/Ym1), human Chi3L1 and Chit1 induce oligodendrogenesis. In mice, Chi3l3 is highly expressed in the subventricular zone, a stem cell niche of the adult brain, and in inflammatory brain lesions during experimental autoimmune encephalomyelitis (EAE). We find that silencing Chi3l3 increases severity of EAE. We present evidence that in NSCs Chi3l3 activates the epidermal growth factor receptor (EGFR), thereby inducing Pyk2-and Erk1/2- dependent expression of a pro-oligodendrogenic transcription factor signature. Our results implicate CLP-EGFR-Pyk2-MEK-ERK as a key intrinsic pathway controlling oligodendrogenesis.







