Summary: Researchers report the gut microbiome could help explain why some people experience toxic side effects from medications. A new study reveals how gut bacteria can transform certain drugs into harmful compounds.
Source: Yale.
People sometimes suffer toxic side effects from drugs that help many others. Yale scientists have identified a surprising explanation — the gut microbiome.
The research, published Feb. 8 in the journal Science, describes how bacteria in the gut can transform three drugs into harmful compounds.
“If we can understand the microbiome’s contributions to drug metabolism, we can decide which drugs to give to patients or even alter the microbiome so patients have a better response,” said co-lead author Michael Zimmermann, postdoctoral fellow in the lab of senior author Andrew Goodman in the Department of Microbial Pathogenesis and the Microbial Sciences Institute.
Goodman, Zimmermann, co-lead author Maria Zimmermann-Kogadeeva, and Rebekka Wegmann, now a doctoral student at ETH Zurich, studied an antiviral drug whose breakdown product can cause severe toxicity and identified how gut microbes transform the drug into a harmful compound. They then administered the drug to mice carrying bacteria engineered to lack this drug-transforming ability and measured the levels of this toxic compound. Using this data, they developed a mathematical model that successfully predicted the role of gut bacteria in metabolizing a second antiviral drug and clonazepam, an anti-seizure and anti-anxiety drug.
The study found that the gut microbes were responsible for producing 20% to 80% of the circulating toxic metabolites derived from the three drugs.
The new model can potentially identify those most at risk of experiencing the side effects of many drugs and help researchers tailor new approaches to minimize this risk to individuals, researchers say.
“Potentially, this approach can be applied to other drugs,” said co-lead author Zimmermann-Kogadeeva, who is also a postdoctoral fellow in the Goodman lab.
Funding: The work was primarily funded by the National Institutes of Health.
Source: Bill Hathaway – Yale
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is adapted from the Yale video.
Video Source: Video credited to Yale.
Original Research: Abstract for “Separating host and microbiome contributions to drug pharmacokinetics and toxicity” by Michael Zimmermann, Maria Zimmermann-Kogadeeva, Rebekka Wegmann, and Andrew L. Goodman in Science. Published February 8 2019.
doi:10.1126/science.aat9931
[cbtabs][cbtab title=”MLA”]Yale”Gut Bacteria May Contribute to Toxic Side Effects of Drugs.” NeuroscienceNews. NeuroscienceNews, 8 February 2019.
<https://neurosciencenews.com/gut-bacteria-drug-toxicity-10714/>.[/cbtab][cbtab title=”APA”]Yale(2019, February 8). Gut Bacteria May Contribute to Toxic Side Effects of Drugs. NeuroscienceNews. Retrieved February 8, 2019 from https://neurosciencenews.com/gut-bacteria-drug-toxicity-10714/[/cbtab][cbtab title=”Chicago”]Yale”Gut Bacteria May Contribute to Toxic Side Effects of Drugs.” https://neurosciencenews.com/gut-bacteria-drug-toxicity-10714/ (accessed February 8, 2019).[/cbtab][/cbtabs]
Abstract
Separating host and microbiome contributions to drug pharmacokinetics and toxicity
INTRODUCTION
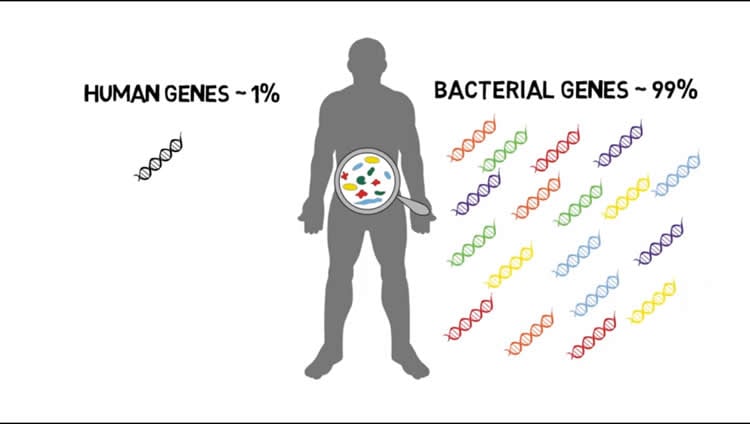
The gut microbiota is implicated in the metabolism of many medical drugs, with consequences for interpersonal variation in drug efficacy and toxicity. However, quantifying microbial contributions to drug metabolism in vivo is challenging, particularly in cases where host and microbiome perform the same metabolic transformation. A quantitative understanding of the physiological, chemical, and microbial factors that determine microbiome contributions to drug metabolism could help explain interpersonal variability in drug response and provide opportunities for personalized medical treatments.
RATIONALE
To experimentally dissect microbiome and host drug metabolism, we combined gut commensal genetics with gnotobiotics to measure metabolism of the nucleoside analog brivudine (BRV) across tissues in mice that vary in a single microbiome-encoded enzyme. Informed by these measurements, we built a pharmacokinetic model to quantitatively predict microbiome contributions to systemic drug and metabolite exposure. Model simulations evaluate the impact of oral bioavailability, host and microbial drug-metabolizing activity, metabolite absorption, and intestinal transit on microbiome contributions to drug metabolism. To test the general applicability of this approach, we performed additional studies with the benzodiazepine clonazepam to quantitatively untangle microbiome contributions to metabolism of a drug subject to multiple metabolic routes and transformations.
RESULTS
We demonstrate BRV conversion to hepatotoxic bromovinyluracil (BVU) by both mammalian and microbial enzymes and reduced systemic BVU exposure in germ-free mice, suggesting a microbiome contribution to serum BVU. Drug conversion assays with axenic cultures and an arrayed transposon library identified BRV-metabolizing gut bacteria and responsible gene products. This enabled us to establish mouse models that are isogenic except for a single bacterial gene responsible for microbial BRV metabolism. Administration of oral BRV and quantification of drug and drug metabolite kinetics in different body compartments provided the data to develop a host-microbiome pharmacokinetic model. This model accurately predicts serum BVU exposure and quantifies host and microbiome contributions to its pharmacokinetics. Model simulations revealed how drug, host, and microbial parameters affect host-microbiome drug metabolism.
To test whether this approach applies to other microbiome-metabolized drugs, we quantified microbiome and host contributions to the metabolism of sorivudine, which is structurally related to BRV but is metabolized to BVU at different rates by both host and microbiome. We also quantified microbiome and host contributions to serum clonazepam metabolites produced through oxidation, nitroreduction, glucuronidation, and enterohepatic cycling.
CONCLUSION
This study provides an experimental and computational strategy to untangle host and microbial contributions to drug metabolism. Quantitative understanding of the interplay between host and microbiome-encoded metabolic activities will clarify how nutritional, environmental, genetic, and galenic factors affect drug metabolism and could enable tailored intervention strategies to improve drug responses. This approach could also be adapted to other xenobiotics, food components, and endogenous metabolites.







