Summary: POMC, a gene which regulates the stress response system, and PER2, a gene associated with circadian regulation, are altered in women who drank moderate-to-high amounts of alcohol during pregnancy and their newborns.
Source: Rutgers
Mothers who drink moderate to high levels of alcohol during pregnancy may be changing their babies’ DNA, according to a Rutgers-led study.
“Our findings may make it easier to test children for prenatal alcohol exposure – and enable early diagnosis and intervention that can help improve the children’s lives,” said lead author Dipak K. Sarkar, a Distinguished Professor and director of the Endocrine Program in the Department of Animal Sciences at Rutgers University-New Brunswick.
The study by Sarkar and scientists in a Collaborative Initiative on Fetal Alcohol Spectrum Disorders is in the journal Alcoholism: Clinical and Experimental Research.
Building on an earlier Rutgers-led study that found binge and heavy drinking may trigger long-lasting genetic change in adults, the researchers sought alcohol-induced DNA changes in 30 pregnant women and 359 children.

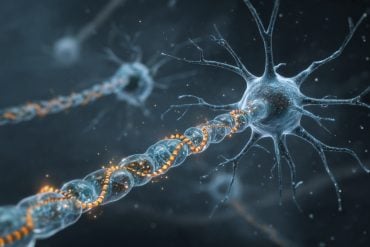
They found changes to two genes – POMC, which regulates the stress-response system, and PER2, which influences the body’s biological clock – in women who drank moderate to high levels of alcohol during pregnancy and in children who had been exposed to those levels of alcohol in the womb.
Heavy drinking in women is four or more drinks on at least five occasions in a month. Moderate drinking in women is about three drinks per occasion.
“Our research may help scientists identify biomarkers – measurable indicators such as altered genes or proteins – that predict the risks from prenatal alcohol exposure,” Sarkar said.
Fetal alcohol spectrum disorders can include physical or intellectual disabilities as well as behavioral and learning problems. While there is no cure, early intervention treatment services can improve a child’s development, according to the U.S. Centers for Disease Control and Prevention, which says there is no known safe amount of alcohol to drink while pregnant.
The study also found that infants exposed to alcohol in the womb – which passes from the mother’s blood through the umbilical cord – had increased levels of cortisol, a potentially harmful stress hormone that can suppress the immune system and lead to ongoing health issues.
Source:
Rutgers
Media Contacts:
Todd Bates – Rutgers
Image Source:
The image is credited to Syani Mukherjee/Rutgers University-New Brunswick.
Original Research: Open access
“Persistent Changes in Stress Regulatory Genes in Pregnant Woman or a Child With Prenatal Alcohol Exposure”. Dipak K. Sarkar et al.
Alcoholism: Clinical and Experimental Research. doi:10.1111/acer.14148
Abstract
Persistent Changes in Stress Regulatory Genes in Pregnant Woman or a Child With Prenatal Alcohol Exposure
Background
We have recently shown that binge or heavy levels of alcohol drinking increase deoxyribonucleic acid (DNA) methylation and reduce gene expression of proopiomelanocortin (POMC) and period 2 (PER2) in adult human subjects (Gangisetty et al., Alcohol Clin Exp Res, 43, 2019, 212). One hypothesis would be that methylation of these 2 genes is consistently associated with alcohol exposure and could be used as biomarkers to predict risk of prenatal alcohol exposure (PAE). Results of the present study provided some support for this hypothesis.
Methods
We conducted a series of studies to determine DNA methylation changes in stress regulatory genes proopiomelanocortin (POMC) and period 2 (PER2) using biological samples from 3 separate cohorts of patients: (i) pregnant women who consumed moderate‐to‐high levels of alcohol or low/unexposed controls, (ii) children with PAE and non–alcohol‐exposed controls, and (iii) children with PAE treated with or without choline.
Results
We found pregnant women who consumed moderate‐to‐high levels of alcohol and gave birth to PAE children had higher DNA methylation of POMC and PER2. PAE children also had increased methylation of POMC and PER2. The differences in the gene methylation of PER2 and POMC between PAE and controls did not differ by maternal smoking status. PAE children had increased levels of stress hormone cortisol and adrenocorticotropic hormone. Choline supplementation reduced DNA hypermethylation and increased expression of POMC and PER2 in children with PAE.
Conclusions
These data suggest that PAE significantly elevates DNA methylation of POMC and PER2 and increases levels of stress hormones. Furthermore, these results suggest the possibility that measuring DNA methylation levels of PER2 and POMC in biological samples from pregnant women or from children may be useful for identification of a woman or a child with PAE.