Cedars-Sinai research suggests that targeting Alzheimer’s disease with specialized immune cells might someday have therapeutic effects in humans.
Cedars-Sinai researchers have successfully tested two new methods for preserving cognition in laboratory mice that exhibit features of Alzheimer’s disease by using white blood cells from bone marrow and a drug for multiple sclerosis to control immune response in the brain.
Under the two approaches, immune cells from outside the brain were found to travel in greater numbers through the blood into the brain. The study showed measurable benefits in mice, an encouraging step toward further testing of these potentially powerful strategies in human trials.
Researchers point out that the brain’s own immune cells are critical for its healthy function. During the progression of Alzheimer’s disease, these cells are found to be defective. In this study, the researchers discovered that immune cells infiltrating the brain from the blood effectively resisted various abnormalities associated with the condition.
“These cells appear to work in the brain in several ways to counter the negative effects associated with Alzheimer’s disease,” said Maya Koronyo-Hamaoui, PhD, assistant professor of neurosurgery and biomedical sciences at Cedars-Sinai, and the senior author of the article published in Brain, a journal of Oxford University Press.
“The increasing incidence of Alzheimer’s disease and the lack of any effective therapy make it imperative to explore new strategies, especially those that can target multiple abnormalities in such a complicated disease,” Koronyo-Hamaoui added.
In Alzheimer’s disease, a protein fragment known as amyloid-beta builds up at the synapses of neurons – the point where neuron-to-neuron communication occurs. As a result, synapses are lost and cognitive function becomes severely impaired.
Immune cells in the brain that are exposed to increasing concentrations of the toxic protein fragment deteriorate and lose their ability to attack and clear away the buildup. Over time, these cells themselves go awry, contributing to harmful inflammation and becoming toxic to the neurons.
During the course of the disease, cells that support the brain’s structure and function also fail at the cellular and molecular levels, steadily impairing memory and learning functions.
In efforts to boost an effective immune response, the Cedars-Sinai scientists have devised ways to “recruit” white blood cells known as monocytes from bone marrow to attack the protein fragments and preserve the synapses.
The researchers evaluated two such methods and their therapeutic potential. In one, they extracted a specific type of monocytes from the bone marrow of healthy young mice and injected the cells into the tail veins of sick mice once a month. A second group of sick mice received weekly under-the-skin injections of glatiramer acetate, an FDA-approved drug used for the treatment of multiple sclerosis; the drug has been shown to foster the migration of white blood cells from the bloodstream to the brain. A third group received both treatments.
All three groups experienced a substantial decrease in Alzheimer’s-like pathology and symptoms.
The varied approaches were effective in “recruiting” protective monocytes to “lesion sites” in the brain, removing protein fragments and reducing harmful inflammation through the secretion of chemicals that regulate immunity at the molecular level, said Koronyo-Hamaoui, the head of Cedars-Sinai’s neuroimmunology laboratory at the Maxine Dunitz Neurosurgical Institute and a faculty member in the Department of Neurosurgery and Department of Biomedical Sciences.
In this study, glatiramer acetate was further found to profoundly affect monocytes’ function, she added.
“This study provides the evidence that a subgroup of unmodified monocytes, extracted from the bone marrow of healthy mouse donors and grafted into the bloodstream, can migrate into the brains of sick mice, directly clear abnormal protein accumulation and preserve cognitive function,” said Yosef Koronyo, the article’s first author and a research associate in the Department of Neurosurgery.
Koronyo added that the study gives unprecedented details about monocyte numbers migrating into brain lesion sites and the compounds they secrete, and shows that the body’s natural monocytes can have direct effects on the integrity of synapses.
Funding: The study was supported by the Coins for Alzheimer’s Research Trust (CART) Fund, the BrightFocus Foundation, the Maurice Marciano Family Foundation, the Saban Family Foundation and the National Center for Advancing Translational Sciences through CTSI grant UL1TR000124. The authors report no competing financial interests.
Source: Sandy Van – Cedars-Sinai
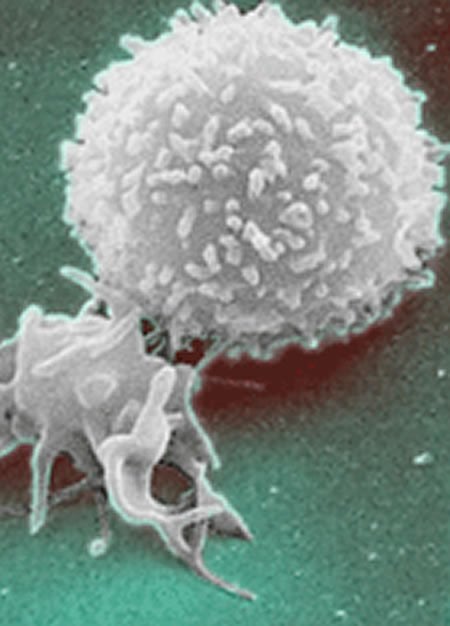
Image Credit: Adapted from a The National Cancer Institute image. This image is in the public domain
Original Research: Abstract for “Therapeutic effects of glatiramer acetate and grafted CD115+ monocytes in a mouse model of Alzheimer’s disease” by Yosef Koronyo, Brenda C. Salumbides, Julia Sheyn, Lindsey Pelissier, Songlin Li, Vladimir Ljubimov, Michelle Moyseyev, David Daley, Dieu-Trang Fuchs, Michael Pham, Keith L. Black, Altan Rentsendorj, and Maya Koronyo-Hamaoui in Brain. Published online June 6 2015 doi:10.1093/brain/awv150
Abstract
Therapeutic effects of glatiramer acetate and grafted CD115+ monocytes in a mouse model of Alzheimer’s disease
Weekly glatiramer acetate immunization of transgenic mice modelling Alzheimer’s disease resulted in retained cognition (Morris water maze test), decreased amyloid-β plaque burden, and regulation of local inflammation through a mechanism involving enhanced recruitment of monocytes. Ablation of bone marrow-derived myeloid cells exacerbated plaque pathology, whereas weekly administration of glatiramer acetate enhanced cerebral recruitment of innate immune cells, which dampened the pathology. Here, we assessed the therapeutic potential of grafted CD115+ monocytes, injected once monthly into the peripheral blood of transgenic APPSWE/PS1ΔE9 Alzheimer’s disease mouse models, with and without weekly immunization of glatiramer acetate, as compared to glatiramer acetate alone. All immune-modulation treatment groups were compared with age-matched phosphate-buffered saline-injected control transgenic and untreated non-transgenic mouse groups. Two independent cohorts of mice were assessed for behavioural performance (6–8 mice/group); treatments started in 10-month-old symptomatic mice and spanned a total of 2 months. For all three treatments, our data suggest a substantial decrease in cognitive deficit as assessed by the Barnes maze test (P < 0.0001–0.001). Improved cognitive function was associated with synaptic preservation and reduction in cerebral amyloid-β protein levels and astrogliosis (P < 0.001 and P < 0.0001), with no apparent additive effects for the combined treatment. The peripherally grafted, green fluorescent protein-labelled and endogenous monocytes, homed to cerebral amyloid plaques and directly engulfed amyloid-β; their recruitment was further enhanced by glatiramer acetate. In glatiramer acetate-immunized mice and, moreover, in the combined treatment group, monocyte recruitment to the brain was coupled with greater elevation of the regulatory cytokine IL10 surrounding amyloid-β plaques. All treated transgenic mice had increased cerebral levels of MMP9 protein (P < 0.05), an enzyme capable of degrading amyloid-β, which was highly expressed by the infiltrating monocytes. In vitro studies using primary cultures of bone marrow monocyte-derived macrophages, demonstrated that glatiramer acetate enhanced the ability of macrophages to phagocytose preformed fibrillar amyloid-β1–42 (P < 0.0001). These glatiramer acetate-treated macrophages exhibited increased expression of the scavenger receptors CD36 and SCARA1 (encoded by MSR1), which can facilitate amyloid-β phagocytosis, and the amyloid-β-degrading enzyme MMP9 (P < 0.0001–0.001). Overall, our studies indicate that increased cerebral infiltration of monocytes, either by enrichment of their levels in the circulation or by weekly immunization with glatiramer acetate, resulted in substantial attenuation of disease progression in murine Alzheimer’s models by mechanisms that involved enhanced cellular uptake and enzymatic degradation of toxic amyloid-β as well as regulation of brain inflammation.
“Therapeutic effects of glatiramer acetate and grafted CD115+ monocytes in a mouse model of Alzheimer’s disease” by Yosef Koronyo, Brenda C. Salumbides, Julia Sheyn, Lindsey Pelissier, Songlin Li, Vladimir Ljubimov, Michelle Moyseyev, David Daley, Dieu-Trang Fuchs, Michael Pham, Keith L. Black, Altan Rentsendorj, and Maya Koronyo-Hamaoui in Brain. Published online June 6 2015 doi:10.1093/brain/awv150






