Summary: Researchers report a potential new drug may reduce the number of brain cells destroyed by stoke and also help repair them.
Source: University of Manchester.
Researchers at The University of Manchester have discovered that a potential new drug reduces the number of brain cells destroyed by stroke and then helps to repair the damage.
A reduction in blood flow to the brain caused by stroke is a major cause of death and disability, and there are few effective treatments.
A team of scientists at The University of Manchester has now found that a potential new stroke drug not only works in rodents by limiting the death of existing brain cells but also by promoting the birth of new neurons (so-called neurogenesis).
This finding provides further support for the development of this anti-inflammatory drug, interleukin-1 receptor antagonist (IL-1Ra in short), as a new treatment for stroke. The drug is already licensed for use in humans for some conditions, including rheumatoid arthritis. Several early stage clinical trials in stroke with IL-1Ra have already been completed in Manchester, though it is not yet licensed for this condition.
In the research, published in the biomedical journal Brain, Behavior and Immunity, the researchers show that in rodents with a stroke there is not only reduced brain damage early on after the stroke, but several days later increased numbers of new neurons, when treated with the anti-inflammatory drug IL-1Ra.
Previous attempts to find a drug to prevent brain damage after stroke have proved unsuccessful and this new research offers the possibility of a new treatment.
Importantly, the use of IL-1Ra might be better than other failed drugs in stroke as it not only limits the initial damage to brain cells, but also helps the brain repair itself long-term through the generation of new brain cells.
Professor Stuart Allan said “The results lend further strong support to the use of IL-1Ra in the treatment of stroke, however further large trials are necessary”.
These new cells are thought to help restore function to areas of the brain damaged by the stroke. Earlier work by the same group showed that treatment with IL-1Ra does indeed help rodents regain motor skills that were initially lost after a stroke. Early stage clinical trials in stroke patients also suggest that IL-1Ra could be beneficial.
The current research is led by Professor Stuart Allan, who commented: “The results lend further strong support to the use of IL-1Ra in the treatment of stroke, however further large trials are necessary.”
Funding: Funding for the research was provided by the Medical Research Council.
Source: University of Manchester
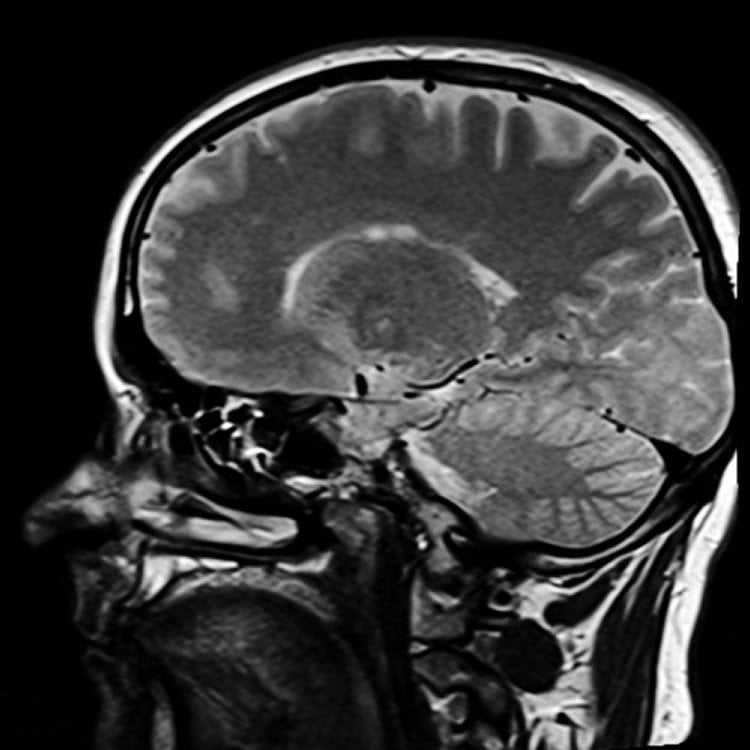
Image Source: This NeuroscienceNews.com image is adapted from the University of Manchester press release.
Video Source: The video is credited to Faculty of Biology, Medicine and Health UoM.
Original Research: Full open access research for “Reparative effects of interleukin-1 receptor antagonist in young and aged/co-morbid rodents after cerebral ischemia” by Jesus M. Pradillo, Katie N. Murray, Graham A. Coutts, Ana Moraga, Fernando Oroz-Gonjar, Herve Boutin, Maria A. Moro, Ignacio Lizasoain, Nancy J. Rothwell, and Stuart M. Allan in Brain, Behavior, and Immunity. Published online November 14 2016 doi:10.1016/j.bbi.2016.11.013
[cbtabs][cbtab title=”MLA”]University of Manchester. “New Drug Limits Then Repairs Brain Damage Caused by Stroke.” NeuroscienceNews. NeuroscienceNews, 26 November 2016.
<https://neurosciencenews.com/stroke-pharmacology-damage-5603/>.[/cbtab][cbtab title=”APA”]University of Manchester. (2016, November 26). New Drug Limits Then Repairs Brain Damage Caused by Stroke. NeuroscienceNews. Retrieved November 26, 2016 from https://neurosciencenews.com/stroke-pharmacology-damage-5603/[/cbtab][cbtab title=”Chicago”]University of Manchester. “New Drug Limits Then Repairs Brain Damage Caused by Stroke.” https://neurosciencenews.com/stroke-pharmacology-damage-5603/ (accessed November 26, 2016).[/cbtab][/cbtabs]
Abstract
Reparative effects of interleukin-1 receptor antagonist in young and aged/co-morbid rodents after cerebral ischemia
Neuroprotective strategies for ischemic stroke have failed to translate from bench to bedside, possibly due to the lack of consideration of key clinical co-morbidities. Stroke and co-morbidities are associated with raised levels of the pro-inflammatory cytokine interleukin-1 (IL-1). Inhibition of IL-1 by the administration of interleukin-1 receptor antagonist (IL-1Ra) has shown to be neuroprotective after experimental cerebral ischemia. Stroke can also trigger a robust neuroreparative response following injury, yet many of these new born neurons fail to survive or integrate into pre-existing circuits. Thus, we explore here effects of IL-1Ra on post-stroke neurogenesis in young and aged/co-morbid rats. Aged lean, aged Corpulent (a model of atherosclerosis, obesity and insulin resistance) and young Wistar male rats were exposed to transient cerebral ischemia, received subcutaneous IL-1Ra 3 and 6 h during reperfusion, and effects on stroke outcome and neurogenesis were analyzed. Our results show that administration of IL-1Ra improves stroke outcome in both young and aged/co-morbid rats. Furthermore, IL-1Ra not only increases stem cell proliferation, but also significantly enhances neuroblast migration and the number of newly born neurons after cerebral ischemia. Overall, our data demonstrate that systemic administration of IL-1Ra improves outcome and promotes neurogenesis after experimental stroke, further highlighting the therapeutic potential of this clinically approved drug.
“Reparative effects of interleukin-1 receptor antagonist in young and aged/co-morbid rodents after cerebral ischemia” by Jesus M. Pradillo, Katie N. Murray, Graham A. Coutts, Ana Moraga, Fernando Oroz-Gonjar, Herve Boutin, Maria A. Moro, Ignacio Lizasoain, Nancy J. Rothwell, and Stuart M. Allan in Brain, Behavior, and Immunity. Published online November 14 2016 doi:10.1016/j.bbi.2016.11.013






