Summary: Oligodendrocyte progenitor cells (OPCs) actively contribute to neuroinflammation associated with multiple sclerosis.
Source: University of Virginia Health System
Cells that scientists have largely ignored when studying multiple sclerosis are actually key contributors to MS development, new research from the University of Virginia School of Medicine shows. The discovery suggests new avenues for devising treatments and is a vital step toward finding a cure.
Understanding Multiple Sclerosis
Scientists had assumed that these cells, known as oligodendrocyte progenitor cells, could only serve a favorable role in MS. These glial cells make up about 5 percent of the brain and spinal cord, and they play an important and beneficial role by making cells that produce myelin – insulation for nerve cells.
In MS, the body’s immune system begins to attack the myelin, leading to a progressively disabling neurological condition that affects more than 2 million people worldwide. (MS is the most common neurological condition among the young, and is often diagnosed between ages 20 and 50.)
It has been thought that these progenitors do not efficiently give rise to myelin-producing cells in people with MS. Yet, UVA’s Alban Gaultier, PhD, and his team made the surprising discovery that they are also actively participating in the immune system’s harmful attacks on myelin.
“This cell type is modulating the inflammatory environment,” said Anthony Fernández-Castañeda, the PhD student who is the first author of the scientific paper outlining the findings. “I was very surprised that these progenitor cells, thought to be a bystander during the inflammatory process, are active contributors to neuroinflammation.”
Promoting Brain Repair
The good news: The new insights into the progenitor cells suggest that doctors could potentially manipulate the environment inside the brain to avoid neurodegeneration and promote brain repair. In the lab, blocking the effects of the cells reduced inflammation and aided in myelin restoration.
“In MS, we have many ways to modulate the initial immune attacks, but we really have no way to promote brain repair,” explained Gaultier, of UVA’s Department of Neuroscience and its Center for Brain Immunology and Glia (BIG). “To come up with a cure, we have to target both aspects of the pathology.”
That will be no easy feat, considering the multiple roles these progenitor cells play. They can’t just be shut down, so scientists would have to develop a more sophisticated approach.
“It’s going to take a lot more work to translate these findings to any form of therapy,” Gaultier said. “We are shining the light on this cell type that very few people have studied as part of the inflammatory response in the brain. More consideration should be given to the varied roles the progenitor cells play when focusing on finding a cure for MS.”
Funding: The research was supported by the National Institutes of Health’s National Institute of Neurological Disorders and Stroke, grants R01 NS083542 and R21 NS111204; the National Multiple Sclerosis Society, grant PP1978; the UVA Double Hoo Research Grant; and the Owens Family Foundation.
Source:
University of Virginia Health System
Media Contacts:
Josh Barney – University of Virginia Health System
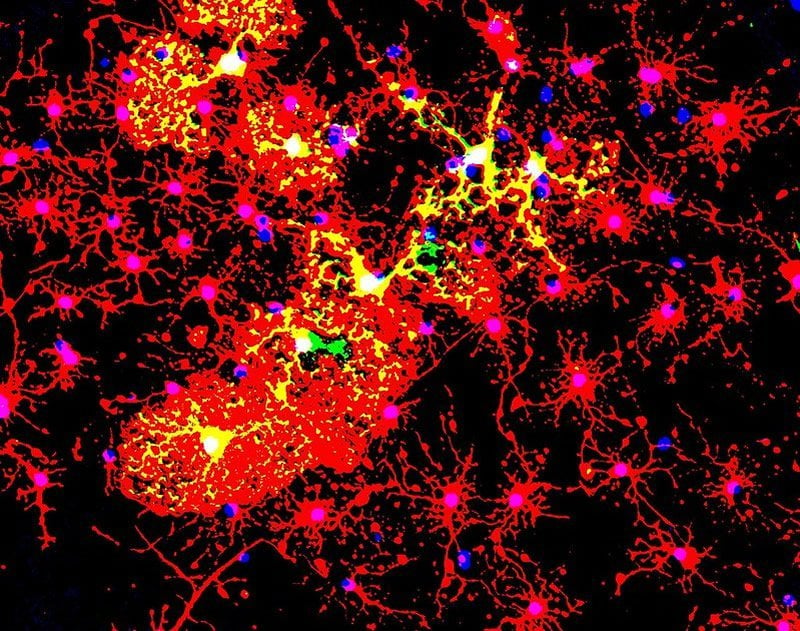
Image Source:
The image is credited to jakeyoung64 licensed CC BY 2.0.
Original Research: Closed access
“The active contribution of OPCs to neuroinflammation is mediated by LRP1”. Anthony Fernández-Castañeda et al.
Acta Neuropathologica doi:10.1007/s00401-019-02073-1.
Abstract
The active contribution of OPCs to neuroinflammation is mediated by LRP1
Oligodendrocyte progenitor cells (OPCs) account for about 5% of total brain and spinal cord cells, giving rise to myelinating oligodendrocytes that provide electrical insulation to neurons of the CNS. OPCs have also recently been shown to regulate inflammatory responses and glial scar formation, suggesting functions that extend beyond myelination. Low-density lipoprotein receptor-related protein 1 (LRP1) is a multifaceted phagocytic receptor that is highly expressed in several CNS cell types, including OPCs. Here, we have generated an oligodendroglia-specific knockout of LRP1, which presents with normal myelin development, but is associated with better outcomes in two animal models of demyelination (EAE and cuprizone). At a mechanistic level, LRP1 did not directly affect OPC differentiation into mature oligodendrocytes. Instead, animals lacking LRP1 in OPCs in the demyelinating CNS were characterized by a robust dampening of inflammation. In particular, LRP1-deficient OPCs presented with impaired antigen cross-presentation machinery, suggesting a failure to propagate the inflammatory response and thus promoting faster myelin repair and neuroprotection. Our study places OPCs as major regulators of neuroinflammation in an LRP1-dependent fashion.