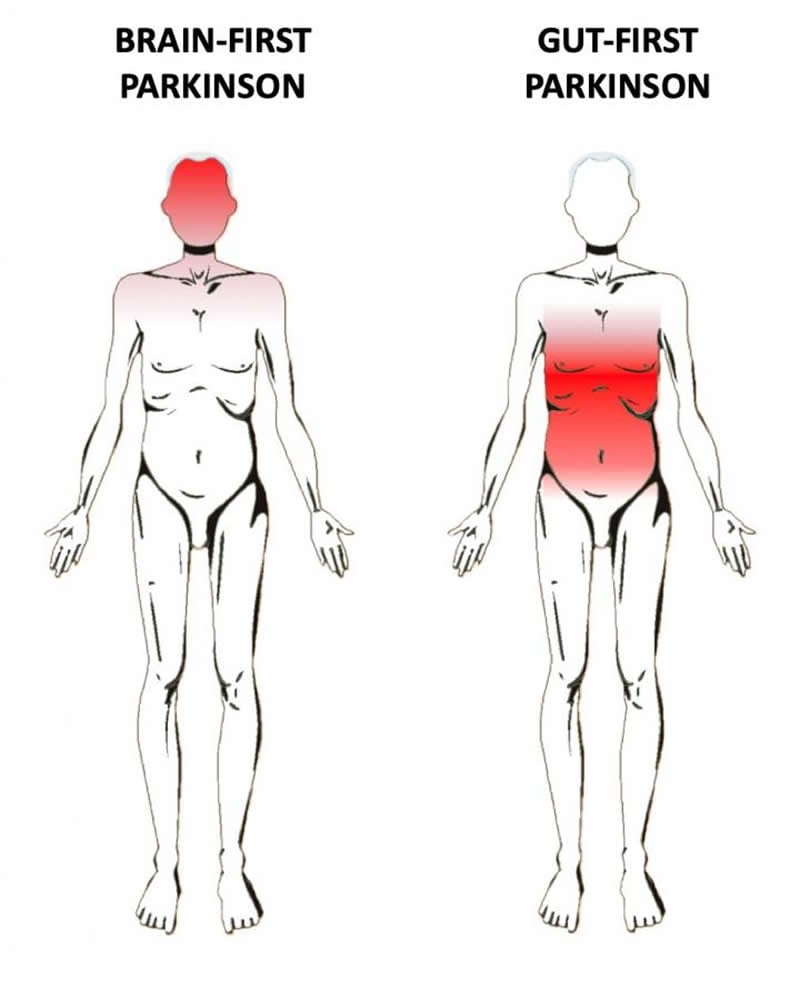
Summary: Lewy body disorders, including Parkinson’s disease and Lewy body dementia, comprise of two distinct subtypes. One subtype originates in the peripheral nervous system (PNS) of the gut and spreads to the brain. The other originates in the brain, or enters the brain via the olfactory system, before spreading to the brainstem and PNS.
Source: IOS Press
Does Parkinson’s disease (PD) start in the brain or the gut? In a new contribution published in the Journal of Parkinson’s Disease, scientists hypothesize that PD can be divided into two subtypes: gut-first, originating in the peripheral nervous system (PNS) of the gut and spreading to the brain; and brain-first, originating in the brain, or entering the brain via the olfactory system, and spreading to the brainstem and peripheral nervous system.
Per Borghammer, MD, PhD, DMSc, Nuclear Medicine & PET, Aarhus University Hospital, Denmark, and Nathalie Van Den Berge, MSc, PhD, Department of Clinical Medicine, Aarhus University, Denmark, explore the origins of PD onset. They review the evidence that Lewy body disorders (LBD), including PD and dementia with Lewy bodies (DLB), comprise two distinct subtypes: (1) a gut-first phenotype in which marked damage to the peripheral autonomic nervous system precedes measurable damage to the brain itself, including the dopamine cells; and (2) a brain-first phenotype, in which marked damage to the brain precedes measurable damage to the peripheral autonomic nervous system.
“Evidence from autopsy studies of brains from PD patients has suggested that PD may start in the peripheral nervous system of the gut and nose. The pathology then spreads via the nerves into the brain. However, not all autopsy studies agree with this interpretation,” explained Dr. Borghammer. “In some cases, the brains do not contain pathology at the important ‘entry points’ into the brain, such as the dorsal vagus nucleus at the bottom of the brainstem. The gut-first versus brain-first hypothesis posited in this review provides a scenario that can reconcile these discrepant findings from the neuropathological literature into one single coherent theory about the origins of PD.”
“The discussion about the origins of PD is often framed as an ‘either-or’, i.e., either all PD cases start in the gut or all cases start in the brain,” added Dr. Van Den Berge. “However, much of the evidence seems compatible with both these interpretations. Thus, we need to entertain the possibility that both scenarios are actually true.”
The review summarizes existing evidence from imaging studies from humans and tissue studies from humans and animal models. The imaging and histology studies are generally compatible with the brain-first vs body-first hypothesis. If this hypothesis is correct, it suggests that PD is more complicated than originally thought. If the disease starts in the gut in only a fraction of patients, it is likely that interventions targeting the gut might only be effective for some PD patients, but not for individuals in which the disease starts in the brain itself.
“If the brain-first vs body-first hypothesis is correct, we need to intensify the research into understanding risk factors and triggering factors for these two subtypes,” noted Dr. Van Den Berge.
“It is probable that these different types of PD need different treatment strategies,” commented Dr. Borghammer. “It may be possible to prevent the ‘gut-first’ type of PD through interventions targeting the gut, such as probiotics, fecal transplants, and anti-inflammatory treatments. However, these strategies might not work with respect to treating and preventing the brain-first type. Thus, a personalized treatment strategy will be required, and we need to be able to identify these subtypes of PD in the individual patient.”
PD is a slowly progressive disorder that affects movement, muscle control and balance. It is the second most common age-related neurodegenerative disorder affecting about three percent of the population by the age of 65 and up to five percent of individuals over 85 years of age. During the 20th century, PD was thought to be primarily a brain disorder characterized mainly by loss of pigmented dopaminergic neurons residing in the substantia nigra, a basal ganglia structure located in the midbrain that plays an important role in reward and movement. More recently, it has become clear that PD is highly varied and probably consists of several subtypes.
Source:
IOS Press
Media Contacts:
Diana Murray – IOS Press
Image Source:
The image is credited to Lundbeck Foundation.
Original Research: Open access
“Brain-First versus Gut-First Parkinson’s Disease: A Hypothesis”. Borghammer, Per and Van Den Berge, Nathalie.
Journal of Parkinson’s Disease doi:10.3233/JPD-191721.
Abstract
Brain-First versus Gut-First Parkinson’s Disease: A Hypothesis
Parkinson’s disease (PD) is a highly heterogeneous disorder, which probably consists of multiple subtypes. Aggregation of misfolded alpha-synuclein and propagation of these proteinacious aggregates through interconnected neural networks is believed to be a crucial pathogenetic factor. It has been hypothesized that the initial pathological alpha-synuclein aggregates originate in the enteric or peripheral nervous system (PNS) and invade the central nervous system (CNS) via retrograde vagal transport. However, evidence from neuropathological studies suggests that not all PD patients can be reconciled with this hypothesis. Importantly, a small fraction of patients do not show pathology in the dorsal motor nucleus of the vagus. Here, it is hypothesized that PD can be divided into a PNS-first and a CNS-first subtype. The former is tightly associated with REM sleep behavior disorder (RBD) during the prodromal phase and is characterized by marked autonomic damage before involvement of the dopaminergic system. In contrast, the CNS-first phenotype is most often RBD-negative during the prodromal phase and characterized by nigrostriatal dopaminergic dysfunction prior to involvement of the autonomic PNS. The existence of these subtypes is supported by in vivo imaging studies of RBD-positive and RBD-negative patient groups and by histological evidence— reviewed herein. The present proposal provides a fresh hypothesis-generating framework for future studies into the etiopathogenesis of PD and seems capable of explaining a number of discrepant findings in the neuropathological literature.






