Summary: Using mouse models, researchers seeded alpha-synuclein aggregates in gut neurons and discovered the clumps can travel to neurons in the brain.
Source: CalTech
Parkinson’s disease (PD) is a debilitating neurodegenerative disorder, impairing the motor functions of millions of elderly people worldwide. Often, people with PD will experience disturbances in gastrointestinal function, such as constipation, years before motor symptoms set in.
Postmortem examinations of the brains of people with PD have shown that their brain cells that control movement are littered with aggregates, or clumps, of a protein called alpha-synuclein (α-Syn). Now, working with mouse models, Caltech researchers have seeded α-Syn aggregates in neurons in the gut and discovered that these clumps can travel up to affect neurons in the brain—but this process depends on age.
Normally, mice produce an enzyme that is able to break down these clumps, but as they get older, they may lose this ability, which could explain why PD develops most often in elderly people. The researchers showed that injecting mice with systemic delivery vectors carrying genes that encode for this enzyme helped ameliorate some of the clumping and partially restored proper gut function.
A paper describing the research appears in the February 17 issue of the journal Nature Neuroscience. The work was led by researchers in the laboratory of Viviana Gradinaru (BS ’05), professor of neuroscience and biological engineering, Heritage Medical Research Institute Investigator, and director of the Center for Molecular and Cellular Neuroscience at the Tianqiao and Chrissy Chen Institute for Neuroscience at Caltech.
As α-Syn aggregates have also been found in neurons in the intestines of people with PD, some researchers hypothesize that α-Syn aggregation begins first in the nervous system of the gut. The idea is that the protein aggregates then hop from neuron to neuron, traveling from the gut nervous system up the vagus nerve and into the brain, seeding the formation of additional aggregates along the way.
“The vagus nerve is a physical connection between neurons in the gut and neurons in the brain. If these damaging protein clusters first originate in gut neurons, then in the future we may be able to diagnose PD earlier and potentially use gene delivery to restore functions to the cells so that they can clean up the aggregates,” says Collin Challis, former postdoctoral scholar and first author on the study.
To test this, the Caltech team injected the gastrointestinal lining of mice with αSyn aggregates and then monitored the aggregates to see if they were progressing up to the brain stem.
In adult mice, the team did find progression of αSyn clusters, but they did not see the development of motor impairments. The αSyn clusters also progressed in elderly mice (about 16 months old), but these mice exhibited both gastrointestinal disturbances—impaired gastric motility and fecal pellet hydration—and motor symptoms.
The question for the team, says Challis, was why these aggregates cause motor disturbances in older mice, whereas younger animals are not affected. “As we get older, we’re not as efficient at dealing with pathogens or misfolded proteins. Parkinson’s disease may be an example of this,” he says.
It was known that the enzyme glucocerebrosidase (GCase) has the ability to break down αSyn clusters. This enzyme is naturally produced by mice—and an analog works similarly in humans—but if a mouse loses the ability to make it, αSyn proteins begin to cluster together.
To study GCase’s effect on PD-related symptoms, the team used mice that were genetically engineered to overproduce αSyn and injected the animals with genes that encode for GCase. These genes were packaged in a variant of adeno-associated virus (AAV), a harmless viral shell that was previously engineered by the Gradinaru lab as a kind of delivery vehicle to get genetic material into gut cells via the bloodstream. The team found that GCase partially restored normal gut function in these mice and decreased the aggregates in gut neurons.
“Mutations in the gene that encodes GCase are responsible for Gaucher disease and a risk factor in PD. Our work shows that this gene can be delivered by AAVs to rescue gastric symptoms in mice, and emphasizes that peripheral neurons are a worthwhile target for treating PD, in addition to the brain,” Gradinaru says.
A paper describing the research is titled “Gut-seeded α-synuclein fibrils promote gut dysfunction and brain pathology specifically in aged mice.” In addition to Challis and Gradinaru, additional co-authors are graduate student Acacia Hori; former postdoctoral scholar Timothy Sampson; graduate student Bryan Yoo; former postdoctoral scholar Rosemary Challis; Adam Hamilton of the Emory University School of Medicine in Atlanta; Sarkis Mazmanian, Luis B. and Nelly Soux Professor of Microbiology and Heritage Medical Research Institute Investigator; and Laura Volpicelli-Daley of the University of Alabama.
Funding: Funding was provided by the National Institutes of Health, the Department of Defense, the Heritage Medical Research Institute, the Pew Charitable Trusts, the Rogers Fellowship for Parkinson’s Research, and the CZI Neurodegeneration Challenge Network. Mazmanian and Gradinaru are affiliated faculty members with the Tianqiao and Chrissy Chen Institute for Neuroscience at Caltech.
Source:
CalTech
Media Contacts:
Lori Dajose – CalTech
Image Source:
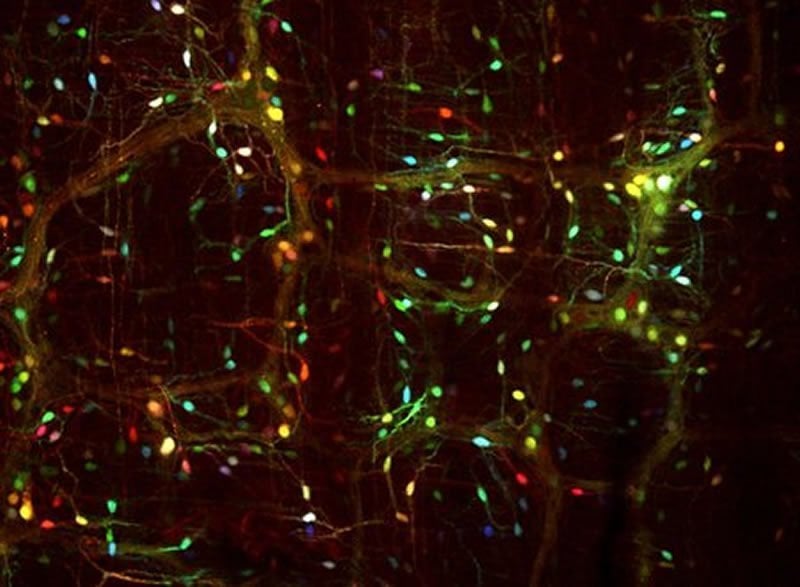
The image is credited to Gradinaru laboratory / Caltech.
Original Research: Closed access
“Gut-seeded α-synuclein fibrils promote gut dysfunction and brain pathology specifically in aged mice”. Collin Challis, Acacia Hori, Timothy R. Sampson, Bryan B. Yoo, Rosemary C. Challis, Adam M. Hamilton, Sarkis K. Mazmanian, Laura A. Volpicelli-Daley & Viviana Gradinaru.
Nature Neuroscience doi:10.1038/s41593-020-0589-7.
Abstract
Gut-seeded α-synuclein fibrils promote gut dysfunction and brain pathology specifically in aged mice
Parkinson’s disease is a synucleinopathy that is characterized by motor dysfunction, death of midbrain dopaminergic neurons and accumulation of α-synuclein (α-Syn) aggregates. Evidence suggests that α-Syn aggregation can originate in peripheral tissues and progress to the brain via autonomic fibers. We tested this by inoculating the duodenal wall of mice with α-Syn preformed fibrils. Following inoculation, we observed gastrointestinal deficits and physiological changes to the enteric nervous system. Using the AAV-PHP.S capsid to target the lysosomal enzyme glucocerebrosidase for peripheral gene transfer, we found that α-Syn pathology is reduced due to the increased expression of this protein. Lastly, inoculation of α-Syn fibrils in aged mice, but not younger mice, resulted in progression of α-Syn histopathology to the midbrain and subsequent motor defects. Our results characterize peripheral synucleinopathy in prodromal Parkinson’s disease and explore cellular mechanisms for the gut-to-brain progression of α-Syn pathology.






