Commonly used antidepressant drugs change levels of a key signaling protein in the brain region that processes both pain and mood, according to a study conducted at the Icahn School of Medicine at Mount Sinai and published August 24 in the Proceedings of the National Academy of Sciences (PNAS). The newly understood mechanism could yield insights into more precise future treatments for nerve pain and depression.
The study was conducted in mice suffering from chronic neuropathic pain, a condition which is caused in mice and humans by nerve damage. Chronic neuropathic pain is often related to diabetes, infection or trauma – and it persists even after the original source of the pain is gone. Past studies have shown that such pain often leads to depression, but brain mechanisms underlying this connection were previously unknown, as were the mechanisms by which common antidepressant drug classes -tricyclic (TCA) antidepressants or Selective Serotonin-Norepinephrine inhibitors (SNRIs) – counter both pain and depression-related symptoms.
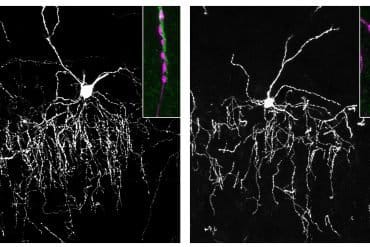
The current study found that the molecular adaptations required for “recovery” from pain and depression are controlled by a gene (RGS9), and the protein it codes for, named RGS9-2. Mice that lacked the gene responsible for encoding RGS9-2 responded much earlier to very low doses of antidepressants, showed significant improvement of sensory deficits and had no signs of depression-related behaviors.
The study suggests that antidepressants that target monoamines, signaling chemicals in the brain that regulate chronic pain and depression, act in the nucleus accumbens, a part of the brain’s reward system, and likely through pathways that pass on messages to nerve cells through RGS9-2.
“Our data reveals that antidepressants that target specific neurotransmitters in the brain, particularly TCAs and SNRIs, regulate chronic pain and depression-related symptoms through actions in the nucleus accumbens,” said Venetia Zachariou, PhD, Associate Professor in the Fishberg Department of Neuroscience and the Friedman Brain Institute, Icahn School of Medicine at Mount Sinai. “We don’t yet know if the typical pain-processing pathways in the spinal cord and the pathways we’ve identified in the brain reward center are directly linked, but we now know more about the cellular pathways that need to be activated in order to achieve pain relief and that effective therapeutics must target both pathways.”

In the treatment of pain, a common course is to treat patients with opioid medications, but these medications show limited effectiveness for neuropathic pain and come with safety and addiction issues. Because antidepressant medications are not addictive, they have become increasingly prescribed to treat neuropathic pain and related depression. Earlier research identified that antidepressants act in the spinal cord to control pain transmission, but little is known about their pain-controlling actions in the brain.
“We found that the molecular pathways required for recovery from neuropathic pain are controlled by RGS9-2,” says Vasiliki Mitsi, a PhD student in the Zachariou lab at the Icahn School of Medicine at Mount Sinai. “In addition, we discovered that by inhibiting RGS9-2, the function of hundreds of other molecules that are important for pain-relief and mood-elevation was boosted,”
The study suggests that therapeutic treatments should target both the brain reward center as well as the previously identified pain-transmitting pathways in the spine. Insight from this study will be used to develop new targets for the treatment of this debilitating disorder.
Funding: This research was supported by the National Institute on Drug Abuse (PPG-POIDAO8227) and the National Institute of Neurological Disorders and Stroke (NS086444).
Source: Elizabeth Dowling – Mount Sinai Hospital
Image Source: The image is credited to NIDA
Original Research: Abstract for “RGS9-2–controlled adaptations in the striatum determine the onset of action and efficacy of antidepressants in neuropathic pain states” by Vasiliki Mitsi, Dimitra Terzi, Immanuel Purushothaman, Lefteris Manouras, Sevasti Gaspari, Rachael L. Neve, Maria Stratinaki, Jian Feng, Li Shen, and Venetia Zachariou in PNAS. Published online August 24 2015 doi:10.1073/pnas.1504283112
Abstract
RGS9-2–controlled adaptations in the striatum determine the onset of action and efficacy of antidepressants in neuropathic pain states
The striatal protein Regulator of G-protein signaling 9-2 (RGS9-2) plays a key modulatory role in opioid, monoamine, and other G-protein–coupled receptor responses. Here, we use the murine spared-nerve injury model of neuropathic pain to investigate the mechanism by which RGS9-2 in the nucleus accumbens (NAc), a brain region involved in mood, reward, and motivation, modulates the actions of tricyclic antidepressants (TCAs). Prevention of RGS9-2 action in the NAc increases the efficacy of the TCA desipramine and dramatically accelerates its onset of action. By controlling the activation of effector molecules by G protein α and βγ subunits, RGS9-2 affects several protein interactions, phosphoprotein levels, and the function of the epigenetic modifier histone deacetylase 5, which are important for TCA responsiveness. Furthermore, information from RNA-sequencing analysis reveals that RGS9-2 in the NAc affects the expression of many genes known to be involved in nociception, analgesia, and antidepressant drug actions. Our findings provide novel information on NAc-specific cellular mechanisms that mediate the actions of TCAs in neuropathic pain states.
“RGS9-2–controlled adaptations in the striatum determine the onset of action and efficacy of antidepressants in neuropathic pain states” by Vasiliki Mitsi, Dimitra Terzi, Immanuel Purushothaman, Lefteris Manouras, Sevasti Gaspari, Rachael L. Neve, Maria Stratinaki, Jian Feng, Li Shen, and Venetia Zachariou in PNAS. Published online August 24 2015 doi:10.1073/pnas.1504283112