Summary: A new study explores the potential link between the gut microbiome and mental health. Researchers report depression may be influenced by disturbances to gut bacteria, suggesting nutrition and diet, in combination with other strategies, could help treat the disorder.
Source: Frontiers.
Researchers continue to explore the role of the gut microbiome in neurodevelopment and mental health.
Better understanding the gastrointestinal microbiome may help psychiatrists treat mental health disorders such as depression, highlights a review in Frontiers in Psychiatry.
From a psychiatric standpoint, the underlying causes of depression are still not fully understood and depression remains difficult to treat in some cases. Given increasing interest in the role of the microbiome in a range of human health issues, this has led many researchers to also investigate potential links between mental health and the microbiome — specifically the microbial flora of the gut.
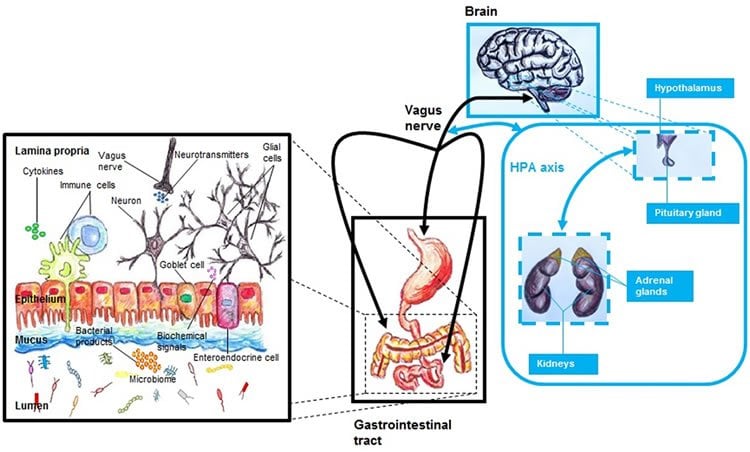
“The main idea of our review is that there is strong communication between the gastrointestinal tract and the brain, and that changes to the microbiome-gut-brain axis could be associated with the etiology of different neuropsychiatric disorders such as depression,” says Juan M. Lima-Ojeda, lead author of the review and a physician and researcher at the University of Regensburg, Germany.
Lima-Ojeda and his colleagues reviewed the body of literature on the role of the gut microbiome with a particular emphasis on the connections, or axis, formed between the microbiome, the gut, and the brain. The brain and the gastrointestinal tract are bi-directionally linked through the central nervous system, endocrine system, and immune system, and perturbations to any of these systems can have repercussions across the others, in turn potentially influencing a person’s overall wellbeing.
“This review was motivated by the interest to obtain a better understanding of both the etiology and pathophysiology of the depressive syndrome,” says Lima-Ojeda. “If we want to improve the treatment strategies that we have for our patients, it is necessary to understand this heterogenic neuropsychiatric disorder.”
Their findings included evidence of the gut-microbiome’s formation and influence beginning already in the very earliest stages of life in-utero. Some of these publications propose that the interactions between the brain and gut are just as influential, if not possibly more important, during neurodevelopment, suggesting that depressive syndromes might be traced back to imbalances during neurodevelopment.
However, Lima-Ojeda additionally uncovered evidence that depression may also be attributable to disturbances to the gut microbiome at any point during a person’s life, which can be due to stress, diet, and of course medications such as antibiotics. These findings promote the idea that attention to nutrition and diet may be a practical and effective complement to existing strategies for the treatment of depression.
“Our habits — including our diet–are important factors modulating the microbiome-gut-brain axis,” says Lima-Ojeda. “So, an appropriate diet is important for adequate mental health, where an appropriate diet is one that includes vegetables, fruits, whole grains, fish, and enough water.”
Funding: This research was funded by German Federal Ministry of Education and Research.
Source: Melissa Cochrane – Frontiers
Image Source: NeuroscienceNews.com image is credited to Lima-Ojeda et al./Frontiers in Psychology.
Original Research: Abstract for ““I Am I and My Bacterial Circumstances”: Linking Gut Microbiome, Neurodevelopment, and Depression” by Juan M. Lima-Ojeda, Rainer Rupprecht and Thomas C. Baghaiin Frontiers in Psychiatry. Published online August 22 2017 doi:10.3389/fpsyt.2017.00153
[cbtabs][cbtab title=”MLA”]Frontiers “Linking Mental Health and the Gut Microbiome.” NeuroscienceNews. NeuroscienceNews, 23 August 2017.
<https://neurosciencenews.com/mental-health-microbiome-7356/>.[/cbtab][cbtab title=”APA”]Frontiers (2017, August 23). Linking Mental Health and the Gut Microbiome. NeuroscienceNew. Retrieved August 23, 2017 from https://neurosciencenews.com/mental-health-microbiome-7356/[/cbtab][cbtab title=”Chicago”]Frontiers “Linking Mental Health and the Gut Microbiome.” https://neurosciencenews.com/mental-health-microbiome-7356/ (accessed August 23, 2017).[/cbtab][/cbtabs]
Abstract
“I Am I and My Bacterial Circumstances”: Linking Gut Microbiome, Neurodevelopment, and Depression
Recently, there has been renewed interest in the role played by microbiome in both human health and human disease. A correct equilibrium between the human host and their microorganisms is important for an appropriate physiological function. Extensive research has shown that microbes that inhabit the gastrointestinal tract—or gut microbiota—are involved not only in both nutritive and digestive activities but also in immunological processes. Moreover, the gut microbiome influences both central nervous system and energy homeostasis. An altered gut microbiome has been associated with the pathophysiology of different diseases, including neuropsychiatric disorders. Apparently, both environmental—diet, exposition to antibiotics, and infections—and host-genetic factors have a strong influence on gut microbiome, modulating the risk for neuropsychiatric illness. Also, early life disruption of the microbiome–gut–brain (MGB) axis has been associated with an increased risk of developing depression later in life, suggesting a link between gut microbiome, neurodevelopment, and depression. This review aims to contribute to this growing area of research by exploring the role played by the gut microbiome in neurodevelopment and in the etiology of the depressive syndrome, including nutritional, immunological, and energy homeostasis approaches.
““I Am I and My Bacterial Circumstances”: Linking Gut Microbiome, Neurodevelopment, and Depression” by Juan M. Lima-Ojeda, Rainer Rupprecht and Thomas C. Baghaiin Frontiers in Psychiatry. Published online August 22 2017 doi:10.3389/fpsyt.2017.00153