Summary: Immune system activation that occurs as result of infection shortly after birth can cause persistent sleep pattern changes and neurodevelopmental disorders, a new study reveals.
Source: McLean Hospital.
McLean Hospital neuroscientists have found that even a brief episode of immune system activation within days of birth can cause persistent changes in sleep patterns concurrent with increases in epilepsy-like brain activity—a combination of symptoms common in autism spectrum disorder (ASD) and other developmental conditions. The detailed findings are available in the January 12, 2018 issue of Neuropsychopharmacology.
“A growing body of evidence suggests that immune system activation, such as that caused by bacterial and viral infections, can play important roles in many brain disorders,” explained Bill Carlezon, PhD, chief of the Division of Basic Neuroscience at McLean Hospital, and senior author of the paper. “While previous research in laboratory animals has established that immune activation during critical prenatal (before birth) developmental periods can later produce the core features of ASD, including decreased social interaction, aberrant communication, and increased repetitive behavior, we wanted to evaluate whether postnatal (during infancy) immune activation could also produce other symptom clusters that are often seen in ASD and related conditions.”
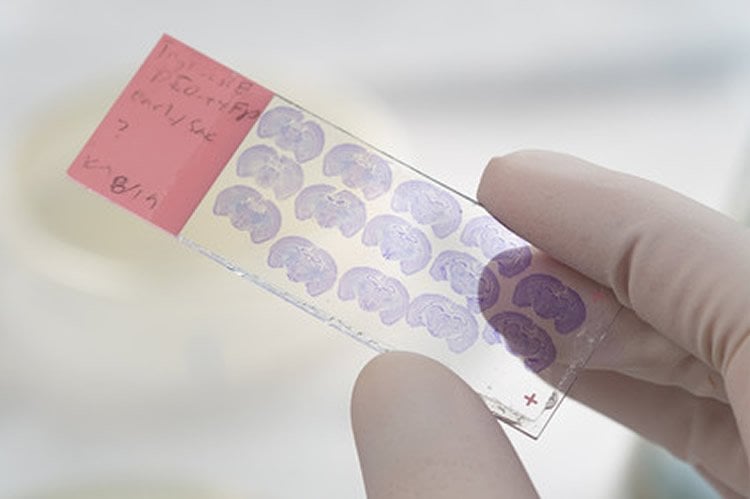
In humans, ASD is also frequently associated with certain co-occurring medical conditions, such as sleep disorders and seizures. To determine whether early postnatal immune system activation can produce these types of effects, McLean researchers treated mice with a lipopolysaccharide (LPS), a chemical that simulates a bacterial infection and causes a temporary (1-3 day) activation of the immune system. The LPS was given at a time point in mice (9 days after birth) that approximates the stage of brain development in humans at birth after full-term pregnancy. The mice were then implanted with micro-transmitters that enabled the researchers to collect an uninterrupted stream of data on sleep, muscle movement, and activity levels. Data collection continued through 12 weeks of age, a time point considered to represent adulthood in mice.
Carlezon, who is a professor of psychiatry at Harvard Medical School, and his team discovered that temporary immune system activation shortly after birth produced two main findings in the adult mice. First, immune-activated mice spent more time in slow-wave sleep, a sleep phase often associated with systemic inflammation. Second, the mice also showed dramatic increases in brief (lasting 2-3 seconds) bouts of abnormal brain wave activity. These events had the hallmark characteristics of spike-wave discharges (SWDs), a type of epilepsy-like brain activity that is not accompanied by full-body seizures. Although the SWDs occurred throughout the day, they were much more prevalent during periods when the mice were sleeping. When they occurred during wakefulness, they were accompanied by complete behavioral arrest—a period of no movement throughout the body—and immediately followed by recovery of normal brain activity and movement. Collectively, these findings demonstrate that even a brief period of immune system activation during critical periods of early development can leave a long-term signature upon the brain.
“The fact that immune system activation can produce these effects on its own, without any type of accompanying injury or trauma, provides new insight on the many paths that can lead to abnormal brain function,” said Carlezon. “While there are clearly other factors that can cause these types of abnormalities, including genetic vulnerabilities, demonstrating that immune activation alone can produce these effects offers new hope for treatments that might reduce their severity, or prevent them altogether, in certain individuals.”
While Carlezon’s research focuses on animal models, his findings have implications for humans. The researchers believe that studying early developmental immune activation in mice may be valuable for diagnosing certain human illnesses and understanding how they develop. Persistent alterations in slow-wave sleep may represent a biomarker that could help differentiate immune-related neuropsychiatric conditions from those with other causes. Meanwhile, understanding epilepsy-like brain activity during both sleep and wakefulness may be useful in developing improved models of ASD. Studies in humans have shown that up to 60% of individuals with ASD experience SWDs during sleep, despite no diagnosis of clinical epilepsy, suggesting accuracy of the mouse model. The SWDs during wakefulness may resemble conditions such as “absence seizures” in humans, which are characterized by a brief loss of consciousness, a blank stare, and cessation of movement, and are often confused with inattention or intellectual disability.
“While more research needs to be conducted, these findings are a significant step forward in unlocking the mystery of ASD and other developmental disorders,” said Carlezon.
Source: Christopher Peterson – McLean Hospital
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is credited to McLean Hospital.
Original Research: Full open access research for “Perinatal Immune Activation Produces Persistent Sleep Alterations and Epileptiform Activity in Male Mice” by Galen Missig, Emery L Mokler, James O Robbins, Abigail J Alexander, Christopher J McDougle & William A Carlezon Jr in Neuropsychopharmacology. Published online October 6 2017 doi:not available
[cbtabs][cbtab title=”MLA”]McLean Hospital “Immune System Activation in Newborns May Affect Developing Brain.” NeuroscienceNews. NeuroscienceNews, 13 January 2018.
<https://neurosciencenews.com/immune-activation-brain-development-8309/>.[/cbtab][cbtab title=”APA”]McLean Hospital (2018, January 13). Immune System Activation in Newborns May Affect Developing Brain. NeuroscienceNews. Retrieved January 13, 2018 from https://neurosciencenews.com/immune-activation-brain-development-8309/[/cbtab][cbtab title=”Chicago”]McLean Hospital “Immune System Activation in Newborns May Affect Developing Brain.” https://neurosciencenews.com/immune-activation-brain-development-8309/ (accessed January 13, 2018).[/cbtab][/cbtabs]
Abstract
Perinatal Immune Activation Produces Persistent Sleep Alterations and Epileptiform Activity in Male Mice
Increasing evidence suggests a role for inflammation in neuropsychiatric conditions, including autism spectrum disorder (ASD). Previous work in rodents has established that immune activation during critical developmental periods can cause phenotypes that reproduce core features of ASD, including decreased social interaction, aberrant communication, and increased repetitive behavior. In humans, ASD is frequently associated with comorbid medical conditions including sleep disorders, motor hyperactivity, and seizures. Here we use a ‘two-hit’ immune-activation paradigm to determine whether perinatal immune activation can also produce these comorbid features in mice. In this paradigm, we treated timed-pregnant mice with polyinosinic:polycytidylic acid (Poly I:C), which simulates a viral infection, on gestational day 12.5 according to an established maternal immune activation regimen. A subset of the offspring also received a second ‘hit’ of lipopolysaccharide (LPS), which simulates a bacterial infection, on postnatal day 9. At 6 weeks of age, mice were implanted with wireless telemetry transmitters that enabled continuous measurements of electroencephalography (EEG), electromyography (EMG), locomotor activity, and subcutaneous temperature. Effects at 7 and 12 weeks of age were compared. Both prenatal Poly I:C and postnatal LPS produced changes in locomotor activity and temperature patterns, increases in slow-wave sleep, and shifts in EEG spectral power, several of which persisted at 12 weeks of age. Postnatal LPS also produced persistent increases in spontaneous bursts of epileptiform activity (spike-wave discharges) that occurred predominantly during sleep. Our findings demonstrate that early-life immune activation can lead to long-lasting physiologic perturbations that resemble medical comorbidities often seen in ASD and other neuropsychiatric conditions.
“Perinatal Immune Activation Produces Persistent Sleep Alterations and Epileptiform Activity in Male Mice” by Galen Missig, Emery L Mokler, James O Robbins, Abigail J Alexander, Christopher J McDougle & William A Carlezon Jr in Neuropsychopharmacology. Published online October 6 2017 doi:not available






