Summary: New research reveals that gut imbalances in children with autism may influence brain activity and behavior by disrupting the production of key neurotransmitters like serotonin. Scientists found that changes in gut-derived metabolites are linked to differences in brain structure and function in children with autism.
This gut-brain communication appears to impact emotional processing and social behaviors, shedding light on why gastrointestinal issues are so common in autism. The study raises the possibility of new therapies that target gut health to alleviate autism-related symptoms.
Key Facts:
- Microbiome-Brain Link: Gut bacteria influence brain activity by affecting tryptophan metabolism and serotonin production.
- Bidirectional Signals: 90% of neural signals between the gut and brain travel from the gut to the brain.
- Autism Impact: Altered gut metabolites correlate with behavioral symptoms and brain activity differences in children with autism.
Source: USC
A new USC study suggests that gut imbalances in children with autism may create an imbalance of metabolites in the digestive system — ultimately disrupting neurotransmitter production and influencing behavioral symptoms.
The research, published Monday in Nature Communications, adds to a growing body of science implicating the “gut-brain” axis in autism.

The discovery raises the possibility of new treatment avenues. It’s an example of how research at USC, and other universities, drives innovation and leads to discoveries that improve lives.
“We demonstrated that gut metabolites impact the brain, and the brain, in turn, affects behavior. Essentially, the brain acts as the intermediary between gut health and autism-related behaviors,” said first author Lisa Aziz-Zadeh, a professor at the Brain and Creativity Institute at the USC Dornsife College of Letters, Arts and Sciences.
“Previous studies highlighted differences in gut microbiomes and brain structures in autism, but our research connects the dots.”
The gut-brain connection is not as far-fetched as it might seem. From an evolutionary perspective, the gut was likely the first “brain,” explained Aziz-Zadeh, who also is a professor at USC Dornsife’s Department of Psychology and the USC Mrs. T.H. Chan Division of Occupational Science and Occupational Therapy.
In fact, most of the neurons from the gut send signals to the brain; there are actually more neurons in the gut than in the spinal cord. About 90% of the neural signals between the gut and brain travel from the gut to the brain, while only 10% go in the opposite direction.
‘Gut instinct’
This constant communication explains why we talk about “gut instinct” or “feeling it in your gut.” Many emotions are processed through gut-related mechanisms, a concept known as interoception — the perception of internal bodily sensations.
For the study, researchers collected behavioral data, brain imaging data and stool samples from 43 children with autism and 41 neurotypical children aged 8-17. From the stool samples, they analyzed metabolites produced by gut bacteria that break down food in the digestive system.
The researchers then correlated these metabolites with brain differences observed in children with autism and their behavioral characteristics.
They homed in on the “tryptophan pathway” by which tryptophan, an amino acid found in many foods, is broken down into several metabolites, including serotonin.
Serotonin is crucial for emotional processing, social interaction, learning and other brain functions. Since much of the body’s serotonin originates in the gut microbiome, changes in gut health can influence serotonin production.
“We know that children with autism have brain differences — certain parts of their brain are either less active or more active compared to typically developing children,” Aziz-Zadeh said.
“We also know they often experience gastrointestinal issues, such as constipation, stomach pain and other digestive problems. Additionally, autism is associated with various symptoms, including repetitive behaviors and social difficulties.”
Sofronia Ringold, a doctoral student at the Brain and Creativity Institute who worked on the study, said she was excited by the possibility of interventions that might target the gut and influence neural activity and behavior “while also hopefully alleviating some of the symptoms that are the most uncomfortable for them.”
In addition to Aziz-Zadeh and Ringold, other authors of the study are Aditya Jayashankar, Emily Kilroy, Ravi Bhatt, and Christiana Butera of USC; and Jonathan Jacobs, Skylar Tanartkit, Swapna Joshi, Mirella Dapretto, Jennifer Labus, and Emeran Mayer, all of UCLA.
Funding: The research was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD079432) and a grant from the Department of Defense’s Idea Development Award (AR170062).
About this microbiome and autism research news
Author: Leigh Hopper
Source: USC
Contact: Leigh Hopper – USC
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Relationships between brain activity, tryptophan-related gut metabolites, and autism symptomatology” by Lisa Aziz-Zadeh, et al. Nature Communications
Abstract
Relationships between brain activity, tryptophan-related gut metabolites, and autism symptomatology
While it has been suggested that alterations in the composition of gut microbial metabolites may play a causative role in the pathophysiology of autism spectrum disorder (ASD), it is not known how gut microbial metabolites are associated with ASD-specific brain alterations.
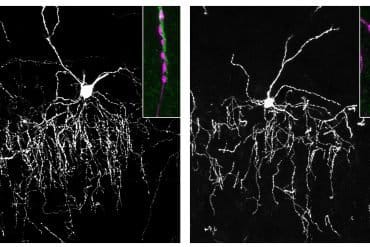
In this cross-sectional, case-control observational study, (i) fecal metabolomics, (ii) task-based functional magnetic resonance imaging (fMRI), and (iii) behavioral assessments were obtained from 43 ASD and 41 neurotypical (NT) children, aged 8–17. The fMRI tasks used socio-emotional and sensory paradigms that commonly reveal strong evoked brain differences in ASD participants.
Our results show that fecal levels of specific tryptophan-related metabolites, including kynurenate, were significantly lower in ASD compared to NT, and were associated with: 1) alterations in insular and cingulate cortical activity previously implicated in ASD; and 2) ASD severity and symptoms (e.g., ADOS scores, disgust propensity, and sensory sensitivities).
Moreover, activity in the mid-insula and mid-cingulate significantly mediated relationships between the microbial tryptophan metabolites (indolelactate and tryptophan betaine) and ASD severity and disgust sensitivity.
Thus, we identify associations between gut microbial tryptophan metabolites, ASD symptoms, and brain activity in humans, particularly in brain regions associated with interoceptive processing.