Summary: A new study in PNAS reports blocking the expression of MDA-9/Syntenin forces glioma stem cells to lose their ability to induce protective autophagy.
Source: Virginia Commonwealth University.
Scientists at Virginia Commonwealth University believe they have uncovered an “Achilles heel” of glioblastoma multiforme (GBM), the most common and deadly form of brain cancer. Their study published this week in the Proceedings of the National Academy of Sciences details how a mechanism that protects glioma stem cells can potentially be exploited to develop new and more effective treatments for GBM.
Autophagy is a process in which cells get rid of unnecessary or dysfunctional components. It can be toxic to the cells, or it can serve a protective role. The researchers demonstrated that protective autophagy allows glioma stem cells to resist anoikis, which is a form of programmed cell death (apoptosis) that occurs when cells detach from the extracellular matrix, or the collection of molecules that helps support and protect cells within the body. The study found that this protective mechanism is regulated by the gene MDA-9/Syntenin.
“We discovered that when we blocked the expression of MDA-9/Syntenin, glioma stem cells lose their ability to induce protective autophagy and succumb to anoikis, resulting in cancer cell death,” says Paul B. Fisher, M.Ph., Ph.D., F.N.A.I., Thelma Newmeyer Corman Endowed Chair in Cancer Research and member of the Cancer Molecular Genetics research program at VCU Massey Cancer Center, chairman of the Department of Human and Molecular Genetics at VCU School of Medicine and director of the VCU Institute of Molecular Medicine. Fisher originally discovered the MDA-9/Syntenin gene, and he and others have shown it to be overexpressed in a majority of cancers.
Fisher, in collaboration with Webster K. Cavenee, Ph.D., Distinguished Professor, Ludwig Institute for Cancer Research, University of California San Diego (UCSD) and other colleagues, found that MDA-9/Syntenin maintains protective autophagy by activating BCL2, a gene that regulates cell death. Additionally, they showed that MDA-9/Syntenin suppresses high levels of autophagy that would be toxic to the cell through epidermal growth factor receptor (EGFR) signaling. Excessive EGFR signaling has been shown to contribute to tumor growth in a wide variety of cancers.
“In the absence of MDA-9/Syntenin, EGFR can no longer maintain protective autophagy. Instead, highly elevated and sustained levels of toxic autophagy ensue that dramatically reduce cancer cell survival,” says Fisher. “This is the first study to define a direct link between MDA-9/Syntenin, protective autophagy and anoikis resistance. We’re hopeful we can exploit this process to develop new and more effective treatments for GBM and possibly other cancers.”
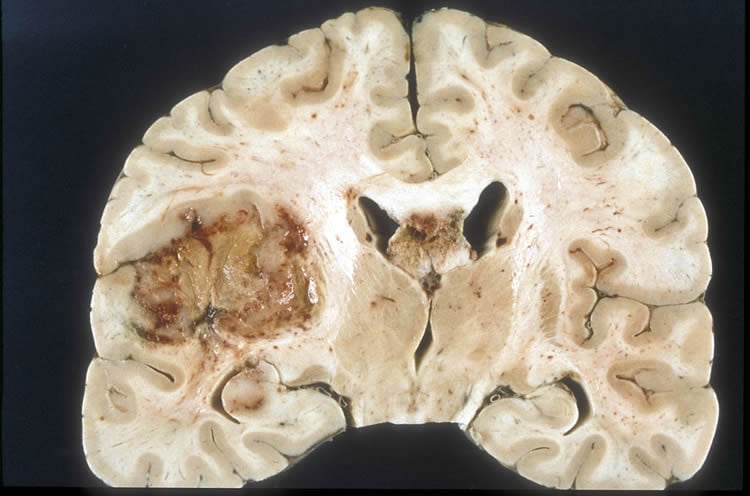
Using GBM cells from patients who underwent surgical removal of their tumors, the scientists demonstrated the loss of these protective biological functions in the absence of MDA-9/Syntenin through laboratory experiments involving glioma stem cell cultures. These findings were then tested in mouse models of human stem cells, where an increase in survival occurred following MDA-9/Syntenin inhibition.
This study builds on an extensive line of research by Fisher and his colleagues into the role of MDA-9/Syntenin in cancer development and progression. Moving forward, they hope to determine if the process they uncovered in this research applies to stem cells from other cancer types. They also plan to continue developing new ways to block the expression of MDA-9/Syntenin. Fisher described one such approach in a recent study demonstrating the effectiveness of an experimental inhibitory drug known as a PDZ1i in reducing MDA-9/Syntenin’s ability to promote invasion of GBM cells in vitro (outside of a living organism) and in vivo (in a living organism).
Fisher collaborated on this research with lead postdoctoral investigator Sarmistha Talukdar, Ph.D., Anjan K. Pradhan, Ph.D., Praveen Bhoopathi, Ph.D., Xue-Ning Shen, M.D., and Laura A. August, all from the Department of Human and Molecular Genetics at VCU School of Medicine; Luni Emdad, M.B.B.S., Ph.D., member of the Cancer Molecular Genetics research program at VCU Massey, assistant professor in the VCU Department of Human and Molecular Genetics and VIMM member; Devanand Sarkar, M.B.B.S., Ph.D., Harrison Research Scholar and member of the Cancer Molecular Genetics research program at VCU Massey, associate professor in the VCU Department of Human and Molecular Genetics and associate scientific director of cancer therapeutics at VIMM; Swadesh K. Das, Ph.D., member of the Cancer Molecular Genetics research program at Massey, assistant professor in the VCU Department of Human and Molecular Genetics and VIMM member; Jolene Windle, Ph.D., Irene Shaw Grigg Distinguished Professor in Genetics Research, co-leader of the Cancer Molecular Genetics research program and resource director of the Transgenic/Knock-out Mouse Facility at Massey as well as professor in the VCU Department of Human and Molecular Genetics and member at VIMM; Frank B. Furnari, Ph.D., professor, and Webster K. Cavenee, Ph.D., distinguished professor, both from the Ludwig Institute for Cancer Research at the University of California San Diego.
Funding: Funding for this study was provided by the National Foundation for Cancer Research, internal funding through the Department of Human and Molecular Genetics at the VCU School of Medicine as well as the VCU Institute of Molecular Medicine, and, in part, by VCU Massey Cancer Center’s NIH-NCI Cancer Center Support Grant P30 CA016059.
Source: John Wallace – Virginia Commonwealth University
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract for “MDA-9/Syntenin regulates protective autophagy in anoikis-resistant glioma stem cells” by Sarmistha Talukdar, Anjan K. Pradhan, Praveen Bhoopathi, Xue-Ning Shen, Laura A. August, Jolene J. Windle, Devanand Sarkar, Frank B. Furnari, Webster K. Cavenee, Swadesh K. Das, Luni Emdad, and Paul B. Fisher in PNAS. Published May 29 2018.
doi:10.1073/pnas.1721650115
[cbtabs][cbtab title=”MLA”]Virginia Commonwealth University “A Potential Achilles Heel in Brain Cancer.” NeuroscienceNews. NeuroscienceNews, 4 June 2018.
<https://neurosciencenews.com/gbm-brain-cancer-genetics-9238/>.[/cbtab][cbtab title=”APA”]Virginia Commonwealth University (2018, June 4). A Potential Achilles Heel in Brain Cancer. NeuroscienceNews. Retrieved June 4, 2018 from https://neurosciencenews.com/gbm-brain-cancer-genetics-9238/[/cbtab][cbtab title=”Chicago”]Virginia Commonwealth University “A Potential Achilles Heel in Brain Cancer.” https://neurosciencenews.com/gbm-brain-cancer-genetics-9238/ (accessed June 4, 2018).[/cbtab][/cbtabs]
Abstract
MDA-9/Syntenin regulates protective autophagy in anoikis-resistant glioma stem cells
Glioma stem cells (GSCs) comprise a small subpopulation of glioblastoma multiforme cells that contribute to therapy resistance, poor prognosis, and tumor recurrence. Protective autophagy promotes resistance of GSCs to anoikis, a form of programmed cell death occurring when anchorage-dependent cells detach from the extracellular matrix. In nonadherent conditions, GSCs display protective autophagy and anoikis-resistance, which correlates with expression of melanoma differentiation associated gene-9/Syntenin (MDA-9) (syndecan binding protein; SDCBP). When MDA-9 is suppressed, GSCs undergo autophagic death supporting the hypothesis that MDA-9 regulates protective autophagy in GSCs under anoikis conditions. MDA-9 maintains protective autophagy through phosphorylation of BCL2 and by suppressing high levels of autophagy through EGFR signaling. MDA-9 promotes these changes by modifying FAK and PKC signaling. Gain-of-function and loss-of-function genetic approaches demonstrate that MDA-9 regulates pEGFR and pBCL2 expression through FAK and pPKC. EGFR signaling inhibits autophagy markers (ATG5, Lamp1, LC3B), helping to maintain protective autophagy, and along with pBCL2 maintain survival of GSCs. In the absence of MDA-9, this protective mechanism is deregulated; EGFR no longer maintains protective autophagy, leading to highly elevated and sustained levels of autophagy and consequently decreased cell survival. In addition, pBCL2 is down-regulated in the absence of MDA-9, leading to cell death in GSCs under conditions of anoikis. Our studies confirm a functional link between MDA-9 expression and protective autophagy in GSCs and show that inhibition of MDA-9 reverses protective autophagy and induces anoikis and cell death in GSCs.






