Summary: A common gut bacterium can trigger antiphospholipid syndrome, an autoimmune disease that affects young women, in those with a genetic predisposition.
Source: Yale
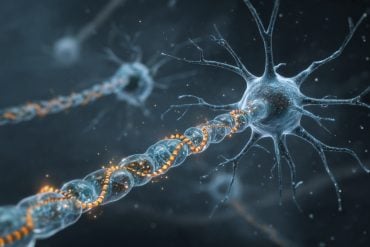
What causes the immune system, designed to protect us, to turn on the body and attack healthy cells? Common bacteria that reside in the human gut may be partly to blame, say Yale researchers, who studied the origins of a serious autoimmune disease that frequently affects young women.
For their study, the research team focused on cells from patients with antiphospholipid syndrome, an immune system disorder that raises the risk of blood clots. This chronic condition can lead to lung clots, strokes, heart attacks, and in pregnant women, miscarriages or stillbirths.
Using patient immune cells and antibodies, as well as animal models of the disease, the investigators did several experiments to explore the phenomenon. They found that a common gut bacterium, Roseburia intestinalis, can trigger the disease in individuals who have a genetic predisposition. In those patients, the immune system’s defender T and B cells react to a blood protein involved in clotting, and also to the bacteria, in certain amino acids found in the bacteria. Over time, this ongoing “cross-reactive” response leads to tissue damage and chronic disease.
By identifying a gut bacterium, instead of the immune system, as the target for treatment, the study could lead to new drugs for these patients, according to the scientists. The research was also the first to show cross-reactivity of gut bacteria in humans with this disease, said senior author Dr. Martin Kriegel of Yale — a finding that could impact the understanding and treatment of other autoimmune diseases.

The full study is published in Cell Host & Microbe.
Other authors are William E. Ruff, Carina Dehner, Woo J. Kim, Odelya Pagovich, Cassyanne L. Aguiar, Andrew T. Yu, Alexander S. Roth, Silvio Manfredo Vieira, Christina Kriegel, Olamide Adeniyi, Melissa J. Mulla, Vikki M. Abrahams, William W. Kwok, Ruth Nussinov, Doruk Erkan, and Andrew L. Goodman.
Funding: This work was supported by grants from the National Institutes of Health (K08AI095318, R01AI118855, T32AI07019, andT32DK007017-39), Yale Rheumatic Diseases Research Core, Women’s Health Research at Yale, O’Brien Center at Yale, Arthritis National Research Foundation, Arthritis Foundation, and Lupus Research Alliance, as well as the American Heart Association, and Lupus Research Institute.
Source:
Yale
Media Contacts:
Ziba Kashef – Yale
Image Source:
The image is credited to Ruff et al, Cell Host Microbe 2019.
Original Research: Closed access
“Pathogenic Autoreactive T and B Cells Cross-React with Mimotopes Expressed by a Common Human Gut Commensal to Trigger Autoimmunity”. Martin Kriegel Perola et al.
Cell Host & Microbe. doi:10.1016/j.chom.2019.05.003
Abstract
Pathogenic Autoreactive T and B Cells Cross-React with Mimotopes Expressed by a Common Human Gut Commensal to Trigger Autoimmunity
Highlights
• Core epitopes of the APS autoantigen β 2GPI are conserved in R. int
• Human β 2GPI-specific Th1 cell clones and autoantibodies cross-react with R. int mimotopes
• Mimotope-dependent anti- R. int titers correlate with anti-β 2GPI titers in APS patients
• Gavage of (NZW × BXSB)F 1 mice with R. int induces anti-β 2GPI IgG and APS-like pathology
Summary
Given the immense antigenic load present in the microbiome, we hypothesized that microbiota mimotopes can be a persistent trigger in human autoimmunity via cross-reactivity. Using antiphospholipid syndrome (APS) as a model, we demonstrate cross-reactivity between non-orthologous mimotopes expressed by a common human gut commensal, Roseburia intestinalis ( R. int), and T and B cell autoepitopes in the APS autoantigen β 2-glycoprotein I (β 2GPI). Autoantigen-reactive CD4 + memory T cell clones and an APS-derived, pathogenic monoclonal antibody cross-reacted with R. int mimotopes. Core-sequence-dependent anti- R. int mimotope IgG titers were significantly elevated in APS patients and correlated with anti-β 2GPI IgG autoantibodies. R. int immunization of mice induced β 2GPI-specific lymphocytes and autoantibodies. Oral gavage of susceptible mice with R. int induced anti-human β 2GPI autoantibodies and autoimmune pathologies. Together, these data support a role for non-orthologous commensal-host cross-reactivity in the development and persistence of autoimmunity in APS, which may apply more broadly to human autoimmune disease.