Summary: Brain inflammation is 30% higher in people with OCD than in their peers without the disorder, a new study reports.
Source: Center for Addiction and Mental Health.
A new brain imaging study by the Centre for Addiction and Mental Health (CAMH) shows for the first time that brain inflammation is significantly elevated – more than 30 per cent higher – in people with obsessive-compulsive disorder (OCD) than in people without the condition. Published today in JAMA Psychiatry, the study provides compelling evidence for a new potential direction for treating this anxiety disorder, which can be debilitating for people who experience it.
“Our research showed a strong relationship between brain inflammation and OCD, particularly in the parts of the brain known to function differently in OCD,” says Dr. Jeffrey Meyer, senior author of the study and Head of the Neuroimaging Program in Mood & Anxiety in CAMH’s Campbell Family Mental Health Research Institute. “This finding represents one of the biggest breakthroughs in understanding the biology of OCD, and may lead to the development of new treatments.”
Inflammation or swelling is the body’s response to infection or injury, and helps the body to heal. But, in some cases, this immune-system response can also be harmful, says Dr. Meyer, who holds a Canada Research Chair in the Neurochemistry of Major Depression. Dampening the harmful effects of inflammation and promoting its curative effects, through new medications or other innovative approaches, could prove to be a new way to treat OCD. In an earlier study, Dr. Meyer discovered that brain inflammation is elevated in people with depression, an illness that can go hand in hand with OCD in some people.
A novel direction for developing treatments is important, since current medications don’t work for nearly one in three people with OCD. About one to two per cent of adolescents and adults have OCD, an anxiety disorder in which people have intrusive or worrisome thoughts that recur and can be hard to ignore.
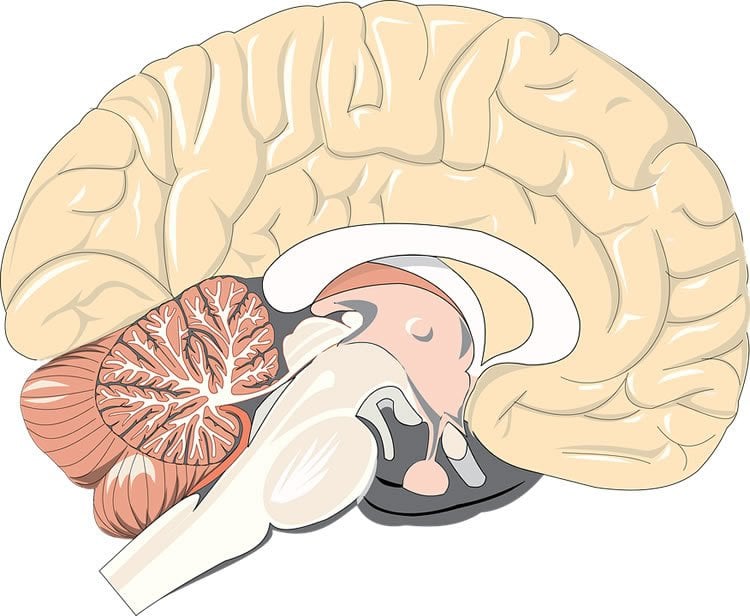
The study included 20 people with OCD and a comparison group of 20 people without the disorder. Doctoral student Sophia Attwells was first author of the study. The researchers used a type of brain imaging called positron emission tomography (PET) that was adapted with special technology at CAMH to see inflammation in the brain. A chemical dye measured the activity of immune cells called microglia, which are active in inflammation, in six brain areas that play a role in OCD. In people with OCD, inflammation was 32 per cent higher on average in these regions. Inflammation was greater in some people with OCD as compared to others, which could reflect variability in the biology of the illness.
Additional investigations are under way to find low-cost blood markers and symptom measures that could identify which individuals with OCD have the greatest level of inflammation and could benefit the most from treatment targeting inflammation. Another notable finding from the current study – a connection between resisting compulsions and brain inflammation – provides one indicator. At least nine out of 10 people with OCD carry out compulsions, the actions or rituals that people do to try to reduce their obsessions. In the study, people who experienced the greatest stress or anxiety when they tried to avoid acting out their compulsions also had the highest levels of inflammation in one brain area. This stress response could also help pinpoint who may best benefit from this type of treatment.
The discovery opens different options for developing treatments. “Medications developed to target brain inflammation in other disorders could be useful in treating OCD,” says Dr. Meyer. “Work needs to be done to uncover the specific factors that contribute to brain inflammation, but finding a way to reduce inflammation’s harmful effects and increase its helpful effects could enable us to develop a new treatment much more quickly.”
Funding: The study was supported by a Canada Research Chair from the Canadian Institutes of Health Research, the Grant family, the Canadian Foundation for Innovation and the Ontario Ministry for Research and Innovation.
Source: Sean O’Malley – Center for Addiction and Mental Health
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Full open access research for “Inflammation in the Neurocircuitry of Obsessive-Compulsive Disorder” by Sophia Attwells, HBSc; Elaine Setiawan, PhD; Alan A. Wilson, PhD; Pablo M. Rusjan, PhD; Romina Mizrahi, MD, PhD, FRCP(C); Laura Miler, HBSc; Cynthia Xu, MD; Margaret Anne Richter, MD, FRCP(C); Alan Kahn, MD, FRCP(C); Stephen J. Kish, PhD; Sylvain Houle, MD, PhD, FRCP(C); Lakshmi Ravindran, MD, FRCP(C); and Jeffrey H. Meyer, MD, PhD, FRCP(C) in JAMA Psychiatry. Published online June 21 2017 doi:10.1001/jamapsychiatry.2017.1567
[cbtabs][cbtab title=”MLA”]Center for Addiction and Mental Health “Human Voices Are Unique But We’re Not That Good at Recognizing Them.” NeuroscienceNews. NeuroscienceNews, 21 June 2017.
<https://neurosciencenews.com/ocd-brain-inflammation-6953/>.[/cbtab][cbtab title=”APA”]Center for Addiction and Mental Health (2017, June 21). Human Voices Are Unique But We’re Not That Good at Recognizing Them. NeuroscienceNew. Retrieved June 21, 2017 from https://neurosciencenews.com/ocd-brain-inflammation-6953/[/cbtab][cbtab title=”Chicago”]Center for Addiction and Mental Health “Human Voices Are Unique But We’re Not That Good at Recognizing Them.” https://neurosciencenews.com/ocd-brain-inflammation-6953/ (accessed June 21, 2017).[/cbtab][/cbtabs]
Abstract
Inflammation in the Neurocircuitry of Obsessive-Compulsive Disorder
Importance For a small percentage of obsessive-compulsive disorder (OCD) cases exhibiting additional neuropsychiatric symptoms, it was proposed that neuroinflammation occurs in the basal ganglia as an autoimmune response to infections. However, it is possible that elevated neuroinflammation, inducible by a diverse range of mechanisms, is important throughout the cortico-striato-thalamo-cortical circuit of OCD. Identifying brain inflammation is possible with the recent advance in positron emission tomography (PET) radioligands that bind to the translocator protein (TSPO). Translocator protein density increases when microglia are activated during neuroinflammation and the TSPO distribution volume (VT) is an index of TSPO density.
Objective To determine whether TSPO VT is elevated in the dorsal caudate, orbitofrontal cortex, thalamus, ventral striatum, dorsal putamen, and anterior cingulate cortex in OCD.
Design, Setting, and Participants This case-control study was conducted at a tertiary care psychiatric hospital from May 1, 2010, to November 30, 2016. Participants with OCD (n = 20) and age-matched healthy control individuals (n = 20) underwent a fluorine F 18–labeled N-(2-(2-fluoroethoxy)benzyl)-N-(4-phenoxypyridin-3-yl)acetamide PET scan. It is a high-quality second-generation TSPO-binding PET radiotracer. All participants were drug and medication free, nonsmoking, and otherwise healthy.
Main Outcomes and Measures The TSPO VT was measured in the dorsal caudate, orbitofrontal cortex, thalamus, ventral striatum, dorsal putamen, and anterior cingulate cortex. Compulsions were assessed with the Yale-Brown Obsessive Compulsive Scale.
Results In the OCD and healthy groups, the mean (SD) ages were 27.4 (7.1) years and 27.6 (6.6) years, respectively, and 11 (55%) and 8 (40%) were women, respectively. In OCD, TSPO VT was significantly elevated in these brain regions (mean, 32%; range, 31%-36% except anterior cingulate cortex, 24%; analysis of variance, effect of diagnosis: P < .001 to P = .004). Slightly lower elevations in TSPO VT (22%-29%) were present in other gray matter regions. The Yale-Brown Obsessive Compulsive Scale measure of distress associated with preventing compulsive behaviors significantly correlated with TSPO VT in the orbitofrontal cortex (uncorrected Pearson correlation r = 0.62; P = .005).
Conclusions and Relevance To our knowledge, this is the first study demonstrating inflammation within the neurocircuitry of OCD. The regional distribution of elevated TSPO VT argues that the autoimmune/neuroinflammatory theories of OCD should extend beyond the basal ganglia to include the cortico-striato-thalamo-cortical circuit. Immunomodulatory therapies should be investigated in adult OCD, rather than solely childhood OCD, particularly in cases with prominent distress when preventing compulsions.
“Memory Reactivation Enables Long-Term Prevention of Interference” by Jasmine Herszage and Nitzan Censor in Current Biology. Published online April 13 2017 doi:10.1016/j.cub.2017.04.025







