Summary: Mouse models of DiGeorge/22q1 Deletion Syndrome reveal a connection between mitochondrial dysfunction, deficits in cortical connectivity and cognitive impairments. Function was restored through antioxidant therapy.
Source: George Washington University
Under-connectivity, or too few connections in the brain, is the underlying cause of brain disorders like autism and schizophrenia, according to a recent study from investigators at the George Washington University (GW) Institute for Neuroscience. The study, published in Neuron, provides the first evidence showing that individual nerve cells fail to make the right number of connections. The reason for this deficit is limited growth of key nerve cells in the cerebral cortex during early development, due to both genetics and mitochondrial dysfunction.
Working in models of DiGeorge/22q11 Deletion Syndrome — a common disorder with the highest known genetic association with diseases like schizophrenia and autism — the GW group defined the disruptions of cell and molecular functions that lead to altered development of nerve cells and their connections in the cerebral cortex. They associated these changes with behavioral deficits linked to neurodevelopmental disorders. This work confirms, for the first time, a well-known clinical hypothesis that under-connectivity is the basis of these disorders.
The work from the GW research team also showed that cortical under-connectivity and cognitive impairment are linked to genes that cause mitochondrial dysfunction in DiGeorge/22q11 Deletion Syndrome. When mitochondrial function is restored through antioxidant therapy, so are cortical connections and behavioral deficits.
“The good news is that mitochondrial deficits are very treatable pharmacologically or through diet” said senior author Anthony-Samuel LaMantia, PhD, director of the GW Institute for Neuroscience and Jeffrey Lieberman Professor of Neurosciences at the GW School of Medicine and Health Sciences. “Our research holds up the possibility that in some instances, children who are diagnosed with neurological disorders may have genetic deficits that lead to a final common pathway of focal metabolic disruption — ultimately, this is treatable.”
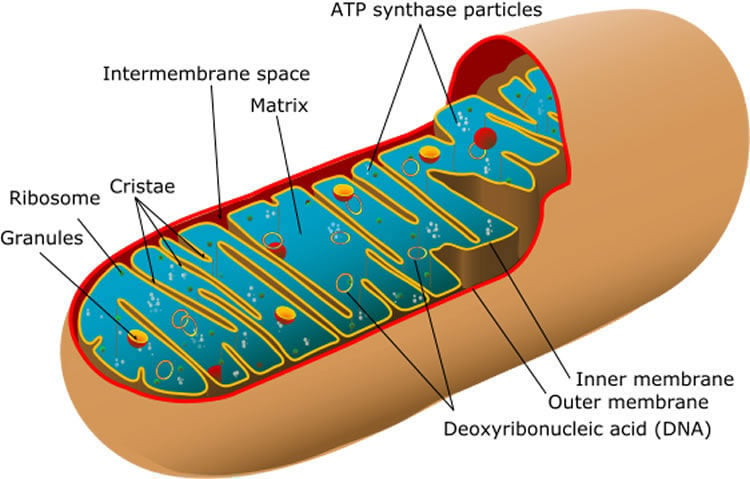
Using a DiGeorge/22q11 Deletion Syndrome mouse model, the GW research team first sought to confirm that under-connectivity, not over-connectivity, underlies behavioral deficits. They found that the integrity and efficiency of synapses in the cortex were diminished. The GW team then looked at the cells making the connections. They found the cells were unhealthy due to dysfunctional mitochondria, long known to be the powerhouse of the cell. The research team then tested the theory that mitochondria in these cells might be dysfunctional due to increased reactive oxygen species — oxygen molecules that roam freely through cells and cause extensive damage. Finally, the team used antioxidant therapy to neutralize these dangerous oxygen “free radicals” to help restore mitochondrial function. This therapy not only fixed connectivity but fixed the behavioral deficits that happened as a result.
The team then looked at the 28 genes on chromosome 22 for which one of two copies is lost in individuals with DiGeorge/22q11 Deletion Syndrome. They focused on six of these 28 genes associated with mitochondria. They identified the Txrnd2 gene, which encodes an enzyme that neutralizes reactive oxygen in mitochondria, as a critical player in the growth and connectivity of the cortical cells that are under-connected.
“This is one of the first times that any group has gone from genetic mutation, to cell biological pathology, to behavioral consequences, and then to safe, effective therapy that corrects both the pathology and behavioral impairment in a valid animal model of any neurodevelopment disorder,” said LaMantia.
In addition to LaMantia, the research included the critical contributions of Alejandra Fernandez, a biomedical PhD candidate in the GW Institute for Biomedical Sciences; Daniel Meechan, senior research scientist in the GW Institute for Neuroscience; Thomas Maynard, PhD, associate professor of anatomy and cell biology at the GW School of Medicine and Health Sciences; Lawrence Rothblat, PhD, research professor of cognitive neuroscience in the Department of Psychology in the GW Columbian College of Arts and Sciences; and Anastas Popratiloff, MD, PhD, director and lead research scientist for the GW Nanofabrication and Imaging Center.
Source:
George Washington University
Media Contacts:
Lisa Anderson – George Washington University
Image Source:
The image is in the public domain.
Original Research: Open access
“Mitochondrial Dysfunction Leads to Cortical Under-Connectivity and Cognitive Impairment”. Anthony-Samuel LaMantia et al.
Neuron. doi:10.1016/j.neuron.2019.04.013
Abstract
Mitochondrial Dysfunction Leads to Cortical Under-Connectivity and Cognitive Impairment
Highlights
• Cortical connections decrease in a DiGeorge/22q11 deletion syndrome mouse model
• Under-connectivity reflects reduced dendrite, axon, and synapse growth
• Txrnd2, a 22q11 gene, regulates mitochondrial metabolism and neuron growth
• Cortical connections and behavioral deficits are restored by anti-oxidant therapy
Summary
Under-connectivity between cerebral cortical association areas may underlie cognitive deficits in neurodevelopmental disorders, including the 22q11.2 deletion syndrome (22q11DS). Using the LgDel 22q11DS mouse model, we assessed cellular, molecular, and developmental origins of under-connectivity and its consequences for cognitive function. Diminished 22q11 gene dosage reduces long-distance projections, limits axon and dendrite growth, and disrupts mitochondrial and synaptic integrity in layer 2/3 but not 5/6 projection neurons (PNs). Diminished dosage of Txnrd2, a 22q11 gene essential for reactive oxygen species catabolism in brain mitochondria, recapitulates these deficits in WT layer 2/3 PNs; Txnrd2 re-expression in LgDel layer 2/3 PNs rescues them. Anti-oxidants reverse LgDel- or Txnrd2-related layer 2/3 mitochondrial, circuit, and cognitive deficits. Accordingly, Txnrd2-mediated oxidative stress reduces layer 2/3 connectivity and impairs cognition in the context of 22q11 deletion. Anti-oxidant restoration of mitochondrial integrity, cortical connectivity, and cognitive behavior defines oxidative stress as a therapeutic target in neurodevelopmental disorders.







