Summary: Scientists sent stem-cell-derived brain organoids to the International Space Station (ISS) to study the effects of microgravity on brain development. After a month in orbit, the organoids remained healthy but displayed accelerated maturation and reduced replication compared to Earth-grown controls.
Gene expression analysis revealed higher levels of genes linked to neuron maturity and lower levels of stress-related inflammation, challenging initial hypotheses. Researchers speculate that microgravity mimics brain-like conditions, offering unique insights into cellular behavior.
These findings could inform research on neurological diseases like Alzheimer’s and Parkinson’s, paving the way for future experiments. The study marks a foundational step in understanding how microgravity impacts brain cells.
Key Facts:
- Accelerated Growth: Brain organoids in microgravity showed faster maturation and reduced proliferation.
- Reduced Stress Response: Contrary to expectations, inflammation and stress-related gene expression were lower in space-grown organoids.
- Future Potential: Insights may help study neurodegenerative diseases and brain cell connectivity under space conditions.
Source: Scripps Research Institute
Microgravity is known to alter the muscles, bones, the immune system and cognition, but little is known about its specific impact on the brain.
To discover how brain cells respond to microgravity, Scripps Research scientists, in collaboration with the New York Stem Cell Foundation, sent tiny clumps of stem-cell derived brain cells called “organoids” to the International Space Station (ISS).
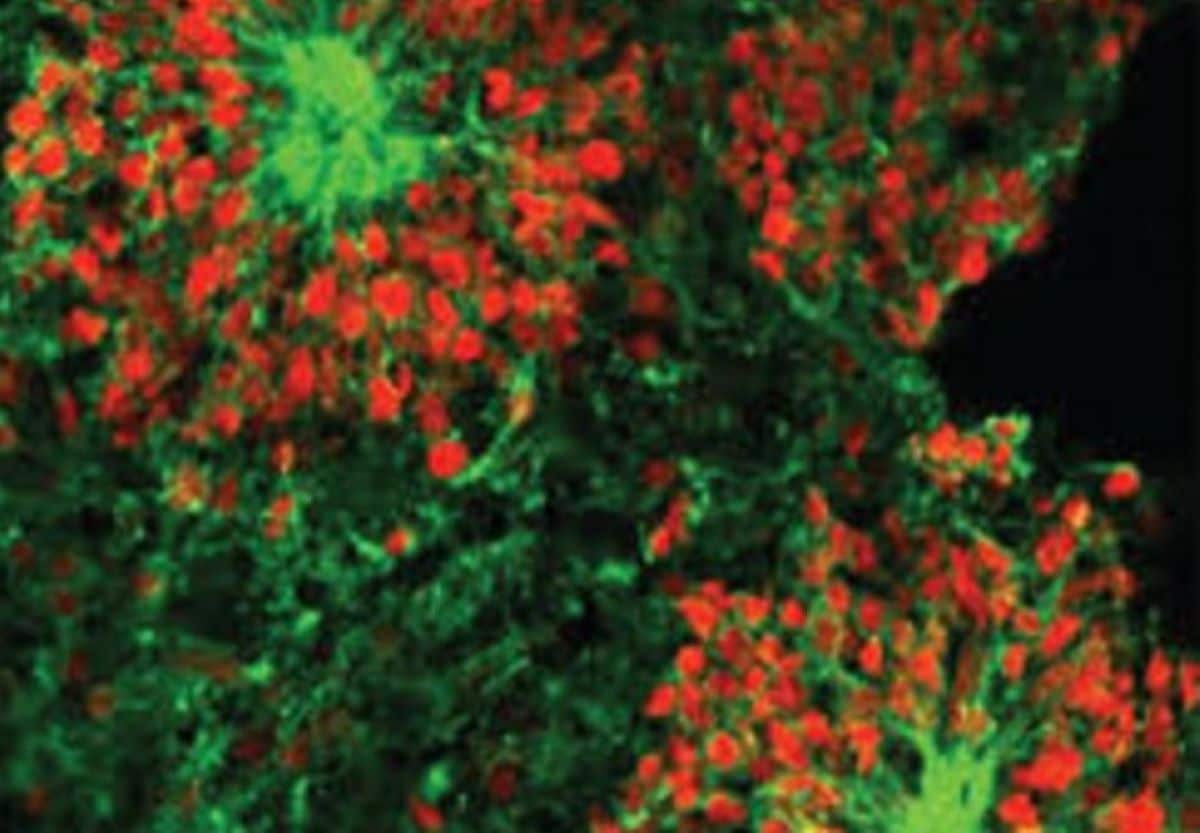
Surprisingly, the organoids were still healthy when they returned from orbit a month later, but the cells had matured faster compared to identical organoids grown on Earth—they were closer to becoming adult neurons and were beginning to show signs of specialization.
The results, which could shed light on potential neurological effects of space travel, were published on October 23, 2024, in Stem Cells Translational Medicine.
“The fact that these cells survived in space was a big surprise,” says co-senior author Jeanne Loring, PhD, professor emeritus in the Department of Molecular Medicine and founding director of the Center for Regenerative Medicine at Scripps Research.
“This lays the groundwork for future experiments in space, in which we can include other parts of the brain that are affected by neurodegenerative disease.”
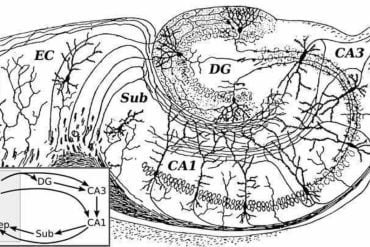
On Earth, the team used stem cells to create organoids consisting of either cortical or dopaminergic neurons, which are the neuronal populations impacted in multiple sclerosis and Parkinson’s disease—diseases that Loring has studied for decades. Some organoids also included microglia, a type of immune cell that is resident within the brain, to examine the impact of microgravity on inflammation.
Organoids are usually grown in a nutrient-rich liquid medium that must be changed regularly to ensure that the cells have adequate nutrition, and to remove waste products. To avoid the need for lab work on the ISS, the team pioneered a method for growing smaller-than-usual organoids in cryovials—small, airtight vials that were originally designed for deep freezing.
The organoids were prepared in labs at the Kennedy Space Station and traveled to the ISS in a miniature incubator. After a month in orbit, they returned to Earth, where the team showed that they were healthy and intact.
To examine how the space environment impacts cellular functions, the team compared the cells’ RNA expression patterns—a measure of gene activity—to identical “ground control” organoids that had remained on Earth.
Surprisingly, they found that the organoids grown in microgravity had higher levels of genes associated with maturity and lower levels of genes associated with proliferation compared to the ground controls, meaning that the cells exposed to microgravity developed faster and replicated less than those on Earth.
“We discovered that in both types of organoids, the gene expression profile was characteristic of an older stage of development than the ones that were on ground,” says Loring.
“In microgravity, they developed faster, but it’s really important to know these were not adult neurons, so this doesn’t tell us anything about aging.”
The team also noted that, contrary to their hypothesis, there was less inflammation and lower expression of stress-related genes in organoids grown in microgravity, but more research is needed to determine why.
Loring speculates that microgravity conditions may more closely mirror the conditions experienced by cells within the brain compared to organoids grown under conventional lab conditions and in the presence of gravity.
“The characteristics of microgravity are probably also at work in people’s brains, because there’s no convection in microgravity—in other words, things don’t move,” says Loring.
“I think that in space, these organoids are more like the brain because they’re not getting flushed with a whole bunch of culture medium or oxygen. They’re very independent; they form something like a brainlet, a microcosm of the brain.”
The paper describes the team’s first space mission, but since then, they have sent four more missions to the ISS. With each one, they’ve replicated the conditions from the first mission and added additional experiments.
“The next thing we plan to do is to study the part of the brain that’s most affected by Alzheimer’s disease,” says Loring.
“We also want to know whether there are differences in the way neurons connect with each other in space. With these kinds of studies, you can’t rely on earlier work to predict what the result would be because there is no earlier work. We’re on the ground floor, so to speak; in the sky, but on the ground floor.”
Funding: This work was supported by funding from the National Stem Cell Foundation.
In addition to Loring, authors of the study, “Effects of microgravity on human iPSC-derived neural organoids on the International Space Station” are Jason Stein of Scripps Research; Davide Marotta, Laraib Ijaz, Lilianne Barbar, Madhura Nijsure, Nicolette Pirjanian, Ilya Kruglikov, Scott A. Noggle, and Valentina Fossati of The New York Stem Cell Foundation Research Institute; Twyman Clements and Jana Stoudemire of Space Tango; and Paula Grisanti of the National Stem Cell Foundation.
About this neuroscience research news
Author: Press Office
Source: Scripps Research Institute
Contact: Press Office – Scripps Research Institute
Image: The image is credited to Jeanne Loring
Original Research: Open access.
“Effects of microgravity on human iPSC-derived neural organoids on the International Space Station” by Jeanne Loring et al. Stem Cells Translational Medicine
Abstract
Effects of microgravity on human iPSC-derived neural organoids on the International Space Station
Research conducted on the International Space Station (ISS) in low-Earth orbit (LEO) has shown the effects of microgravity on multiple organs. To investigate the effects of microgravity on the central nervous system, we developed a unique organoid strategy for modeling specific regions of the brain that are affected by neurodegenerative diseases.
We generated 3-dimensional human neural organoids from induced pluripotent stem cells (iPSCs) derived from individuals affected by primary progressive multiple sclerosis (PPMS) or Parkinson’s disease (PD) and non-symptomatic controls, by differentiating them toward cortical and dopaminergic fates, respectively, and combined them with isogenic microglia.
The organoids were cultured for a month using a novel sealed cryovial culture method on the International Space Station (ISS) and a parallel set that remained on Earth. Live samples were returned to Earth for analysis by RNA expression and histology and were attached to culture dishes to enable neurite outgrowth.
Our results show that both cortical and dopaminergic organoids cultured in LEO had lower levels of genes associated with cell proliferation and higher levels of maturation-associated genes, suggesting that the cells matured more quickly in LEO.
This study is continuing with several more missions in order to understand the mechanisms underlying accelerated maturation and to investigate other neurological diseases.
Our goal is to make use of the opportunity to study neural cells in LEO to better understand and treat neurodegenerative disease on Earth and to help ameliorate potentially adverse neurological effects of space travel.