Summary: Immune cells can accelerate the growth of cancerous tumors in mouse models of NF1.
Source: WUSTL
Tumors arise when cells shake off their restraints and start to multiply out of control. But how fast a tumor grows does not depend solely on how quickly the cancer cells can divide, a new study has found
By examining brain tumors in mice, researchers at Washington University School of Medicine in St. Louis discovered that immune cells that should be defending the body against disease sometimes can be enticed into providing aid and comfort to tumor cells instead. The more immune cells a tumor can recruit to its side, the faster the tumor grows, the researchers found.
The findings, published May 29 in the journal Neuro-Oncology, suggest that targeting immune system cells could potentially slow brain tumor growth in people with the genetic condition neurofibromatosis type 1 (NF1).
“It’s not just all about the tumor cell anymore,” said senior author David H. Gutmann, MD, PhD, the Donald O. Schnuck Family Professor of Neurology and director of the Washington University Neurofibromatosis Center. “It’s also about what happens in the tumor environment that drives brain cancer growth. This gives us another way to attack these tumors beyond merely killing the cancer cells – namely, interrupting the communication between tumor cells and immune system cells.”
While people with NF1 usually come to medical attention for birthmarks on their skin, they are also at increased risk of developing tumors. One of the most common of these tumors in children is a low-grade brain tumor called an optic glioma, which affects the optic nerve that connects the brain and the eye. Some of these tumors can cause vision loss.
Unfortunately, NF1 is a notoriously variable disease. Doctors can’t predict what kinds of tumors a person will develop, how fast these tumors will grow, or what types of medical problems the tumors will cause – all of which make it difficult for doctors to decide when a tumor needs to be treated with chemotherapy and when it is safe to simply watch and wait.
To better understand why some tumors grow faster than others, first author Xiaofan Guo, MD, a graduate student in Gutmann’s research laboratory, created five mouse strains with different genetic changes in the NF1 gene and elsewhere in the mouse’s genome.
The five strains varied widely in tumor development and growth. Mice belonging to three of the strains grew tumors starting at about 3 months of age, with the tumors in one strain of mice growing particularly fast. Members of the fourth strain didn’t grow tumors until they were about 6 months old, and only a quarter of mice in the fifth strain developed brain tumors on the optic nerve at all.

When the researchers isolated tumor cells from the mice and grew them in a dish, they found little difference in tumor cell growth. The growth rates and other properties of the cancer cells were very similar, no matter which mutation the tumor cells carried.
What did correlate with overall tumor proliferation in mice was the presence of two kinds of immune cells – microglia and T cells – within the tumors. Guo and former postdoctoral research fellow Yuan Pan, PhD, discovered that the tumor cells themselves were releasing immune system proteins that attracted immune cells to the tumor.
“Cells that should be part of the brain’s defense against tumors have become part of the process of making and growing a tumor,” said Gutmann, who is also a professor of genetics, of neurological surgery and of pediatrics.
The researchers now are trying to take advantage of this relationship between tumor cells and immune system cells to find new ways to treat brain tumors in people with NF1. One strategy is to slow tumor growth by preventing microglia or T cells from providing support to the cancer cells. However, a more ambitious strategy is to reprogram the T cells to no longer aid tumor cell growth.
“The idea is to use T cells as Trojan horses,” Gutmann said. “These are experiments currently ongoing: We’re trying to change the T cells so that when they enter the brain, instead of promoting the tumor, they shut it down.”
Source:
WUSTL
Media Contacts:
Judy Martin Finch – WUSTL
Image Source:
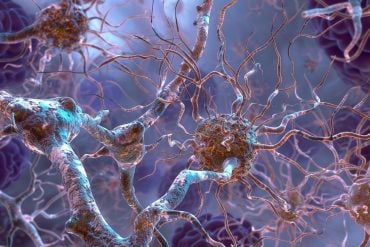
The image is credited to Washington University.
Original Research: Closed access
“Genetic and genomic alterations differentially dictate low-grade glioma growth through cancer stem cell–specific chemokine recruitment of T cells and microgliae”. Xiaofan Guo, Yuan Pan, David H Gutmann.
Neuro-Oncology. doi:10.1093/neuonc/noz080
Abstract
Genetic and genomic alterations differentially dictate low-grade glioma growth through cancer stem cell–specific chemokine recruitment of T cells and microglia
Background
One of the clinical hallmarks of low-grade gliomas (LGGs) arising in children with the neurofibromatosis type 1 (NF1) cancer predisposition syndrome is significant clinical variability with respect to tumor growth, associated neurologic deficits, and response to therapy. Numerous factors could contribute to this clinical heterogeneity, including the tumor cell of origin, the specific germline NF1 gene mutation, and the coexistence of additional genomic alterations. Since human specimens are rarely acquired, and have proven difficult to maintain in vitro or as xenografts in vivo, we have developed a series of Nf1 mutant optic glioma mouse strains representing each of these contributing factors.
Methods
Optic glioma stem cells (o-GSCs) were generated from this collection of Nf1 genetically engineered mice, and analyzed for their intrinsic growth properties, as well as the production of chemokines that could differentially attract T cells and microglia.
Results
The observed differences in Nf1 optic glioma growth are not the result of cell autonomous growth properties of o-GSCs, but rather the unique patterns of o-GSC chemokine expression, which differentially attract T cells and microglia. This immune profile collectively dictates the levels of chemokine C-C ligand 5 (Ccl5) expression, the key stromal factor that drives murine Nf1 optic glioma growth.
Conclusions
These findings reveal that genetic and genomic alterations create murine LGG biological heterogeneity through the differential recruitment of T cells and microglia by o-GSC–produced chemokines, which ultimately determine the expression of stromal factors that drive tumor growth.