Summary: Hepatitis C virus increases the expression of SOCS, dulling the normal immune system response to viral infections. This may explain why Hepatitis C ‘hides’ in the immune system, leading to a lack of diagnosis in those suffering the infection.
Source: TCD
Scientists from Trinity College Dublin have discovered how the highly infectious and sometimes deadly Hepatitis C virus (HCV) “ghosts” our immune system and remains undiagnosed in many people. They report their findings in the international FASEB journal.
HCV’s main route of transmission is via infected blood but over the past 40 years, it has accidentally been given to many patients across the world via infected blood products. The virus replicates particularly well in the liver, and the damage it causes makes it a leading cause of liver disease worldwide.
Even though HCV can be deadly, initial infection is rarely accompanied by any obvious clinical symptoms for reasons that have – until now – remained unknown. As a result, it often goes undiagnosed for the first 6-12 months following infection.
If left untreated HCV spreads throughout the liver, stimulating a low-level inflammatory response. Over several months, these mild responses – accompanied by subsequent liver repair – result in fibrotic scarring of the liver. The liver’s main job is to filter out toxins, but during HCV infection the build-up of fibrotic, non-functioning liver tissue, results in reduced liver function. Without a fully functioning liver, one major side-effect is the build-up of toxins, often referred to as “jaundice”. If patients do not realise they are infected with HCV, their first noticeable symptoms are the side-effects of liver fibrosis (such as jaundice).
While the majority of HCV infections are now treatable with new medicines, early detection would avoid the damaging progression to liver disease. Therefore, a group of scientists led by Assistant Professor in Immunology at Trinity, Nigel Stevenson, set out to understand how the virus avoids being discovered for months after infection.
HCV suppresses the immune response
Under normal circumstances, our cells communicate with each other with molecules called cytokines, which work by activating specific cascades of other molecules within our cells called signalling pathways. These cytokines and their signalling pathways trigger the expression of hundreds of molecules within our cells to increase inflammation and anti-viral activity. This immune response is capable of killing and clearing viral infections from our cells and bodies.
Uncontrolled inflammation would be dangerous, however, so to ensure our immune response to infection is appropriately regulated, several cytokine signalling pathways are controlled by immune regulators called “Suppressor Of Cytokine Signalling (SOCS)” regulators. After a period of time following an initial response, pro-inflammatory cytokine signalling pathways are shut down by SOCS.
The Trinity scientists found that HCV “ghosts” our immune response, by triggering our own SOCS regulators; a specific part of the virus is responsible for increasing a specific SOCS molecule – in both liver and immune cells.
Dr Stevenson said: “We’ve discovered that HCV hijacks this regulatory process by causing the expression of SOCS in our cells. By increasing the expression of SOCS, HCV basically dulls the normal immune response to viral infection. Without a strong signal, our body’s cells cannot then mount an effective inflammatory and anti-viral response that clears the infection.”
“This ability shields HCV from our body’s normal, effective anti-viral immune response and creates a perfect environment in which to survive, replicate and infect other cells. Many diseases are mediated by increasing the inflammatory response to an inappropriately high level, but in this case it is the lack of adequate inflammation that enables HCV to go undiagnosed, leaving it free to rapidly replicate and infect other cells.”
Source:
TCD
Media Contacts:
Thomas Deane – TCD
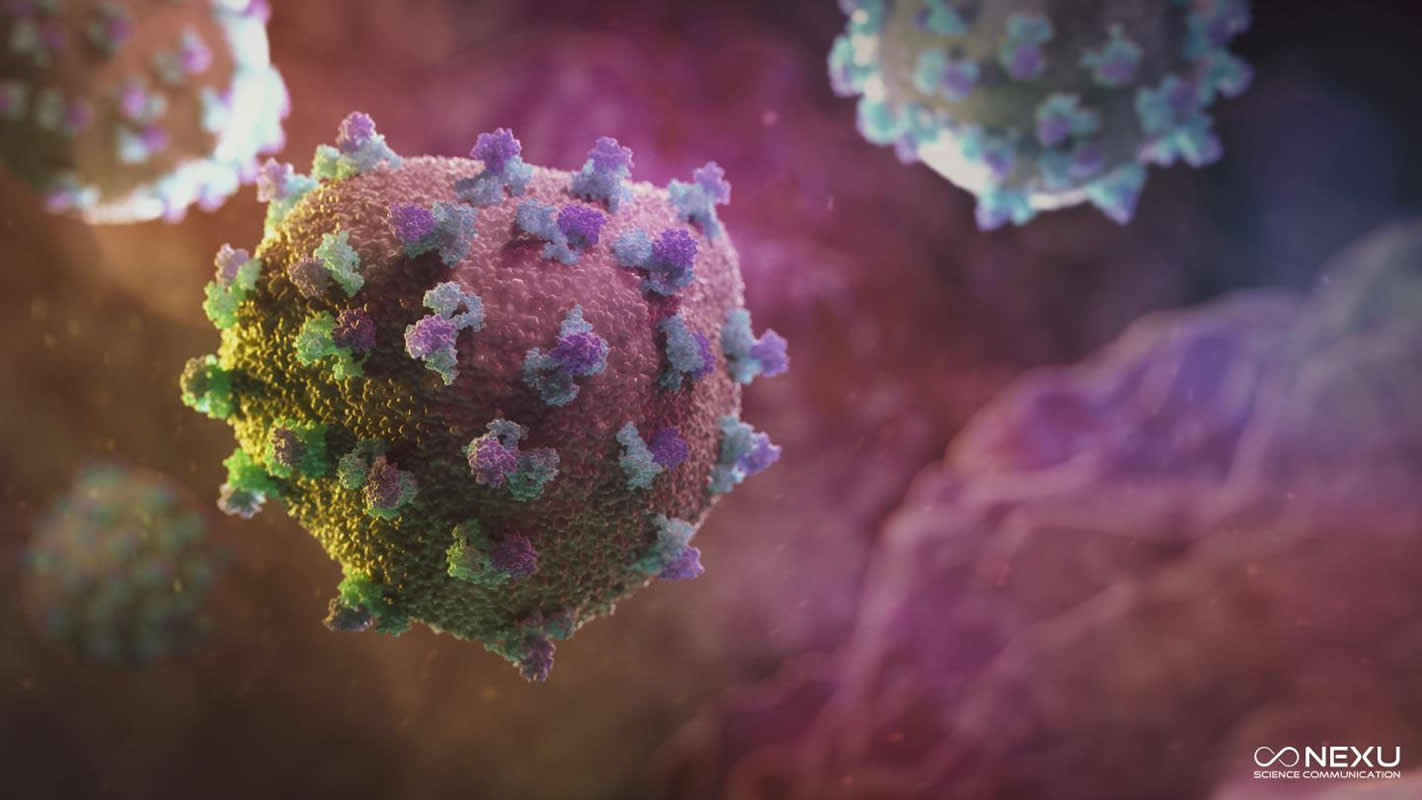
Image Source:
The image is credited to Nexu Science Communication.
Original Research: Closed access
“The hepatitis C virus (HCV) protein, p7, suppresses inflammatory responses to tumor necrosis factor (TNF)-α via signal transducer and activator of transcription (STAT)3 and extracellular signal-regulated kinase (ERK)–mediated induction of suppressor of cytokine signaling (SOCS)3”. Orla Convery, Siobhan Gargan, Michelle Kickham, Martina Schroder, Cliona O’Farrelly, and Nigel J. Stevenson.
FASEB Journal. doi:10.1096/fj.201800629RR
Abstract
The hepatitis C virus (HCV) protein, p7, suppresses inflammatory responses to tumor necrosis factor (TNF)-α via signal transducer and activator of transcription (STAT)3 and extracellular signal-regulated kinase (ERK)–mediated induction of suppressor of cytokine signaling (SOCS)3
Viruses use a spectrum of immune evasion strategies that enable infection and replication. The acute phase of hepatitis C virus (HCV) infection is characterized by nonspecific and often mild clinical symptoms, suggesting an immunosuppressive mechanism that, unless symptomatic liver disease presents, allows the virus to remain largely undetected. We previously reported that HCV induced the regulatory protein suppressor of cytokine signaling (SOCS)3, which inhibited TNF-α–mediated inflammatory responses. However, the mechanism by which HCV up-regulates SOCS3 remains unknown. Here we show that the HCV protein, p7, enhances both SOCS3 mRNA and protein expression. A p7 inhibitor reduced SOCS3 induction, indicating that p7’s ion channel activity was required for optimal up-regulation of SOCS3. Short hairpin RNA and chemical inhibition revealed that both the Janus kinase–signal transducer and activator of transcription (JAK-STAT) and MAPK pathways were required for p7-mediated induction of SOCS3. HCV-p7 expression suppressed TNF-α–mediated IκB-α degradation and subsequent NF-κB promoter activity, revealing a new and functional, anti-inflammatory effect of p7. Together, these findings identify a molecular mechanism by which HCV-p7 induces SOCS3 through STAT3 and ERK activation and demonstrate that p7 suppresses proinflammatory responses to TNF-α, possibly explaining the lack of inflammatory symptoms observed during early HCV infection.—Convery, O., Gargan, S., Kickham, M., Schroder, M., O’Farrelly, C., Stevenson, N. J. The hepatitis C virus (HCV) protein, p7, suppresses inflammatory responses to tumor necrosis factor (TNF)-α via signal transducer and activator of transcription (STAT)3 and extracellular signal-regulated kinase (ERK)–mediated induction of suppressor of cytokine signaling (SOCS)3.







