Summary: According to researchers, gut serotonin levels are doubled in obese people. Researchers report obesity may be characterized by an increased capacity to release and produce serotonin in the gut.
Source: University of Adelaide.
The key chemical for happiness and sadness, serotonin, is also a force in our body’s weight gain and calorie control, and scientists say more research could reduce obesity rates.
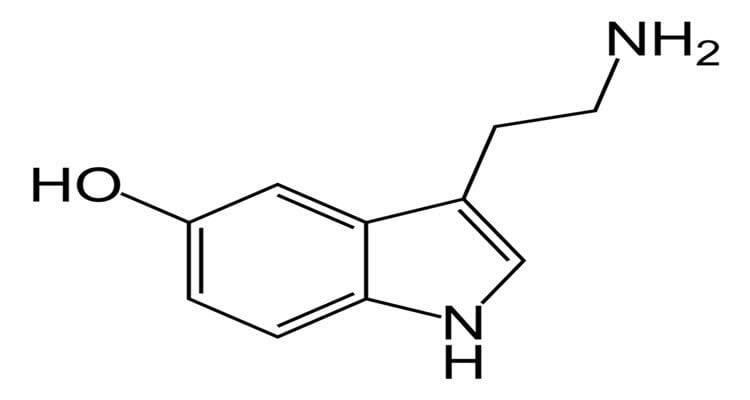
In a new development in gastrointestinal research, researchers from Flinders University, SAHMRI and the University of Adelaide have found more evidence that elevated concentrations of serotonin, the crucial neurotransmitter that chemically transmits messages to nerve cells in the body, is also linked to obesity.
Only recently have researchers understood that this “gut serotonin” is actually bad for our metabolism, as it increases blood glucose and fat mass, thus endangering us of developing diabetes and obesity.
The new research demonstrates for the first time in humans that this gut serotonin is doubled in obese individuals. This new insight now paves the way to try and find potential new treatments for obesity by focusing on the cells in our gut that produce this hormone.
The South Australian researchers were part of a large international research team including University of Adelaide experts that found human obesity is characterised by an increased capacity to produce and release serotonin in the gut.
Their findings are catalogued in the article titled ‘Augmented capacity for peripheral serotonin release in human obesity’, which has been published in the International Journal of Obesity.
“Our gut wall is lined by a protective layer of cells similar to skin cells. But scattered amongst these exists a variety of hormone-producing cells that play important roles in controlling our metabolism, fat mass, and even telling our brain when to stop or start eating,” says Professor Keating, NHMRC Research Fellow Professor Damien Keating, from Flinders University and the South Australian Health and Medical Research Institute (SAHMRI)..
“Half of these cells produce serotonin, which is most commonly associated with having important roles in the brain to make us feel happy. However more than 90% of our bodies serotonin is actually made in the gut, which cannot enter the brain to affect mood.
“We know from a raft of recent high profile publications that gut-derived serotonin causes diabetes and obesity, but we didn’t know if this was relevant to such disorders in humans. Our findings are the first work implicating serotonin as a driver of worsening obesity in humans,” says Professor Keating.
“Having established this, we can now focus on understanding why this happens, so we can develop methods to reduce circulating serotonin levels. These sorts of therapeutic outcomes are exactly why Pfizer decided to partner with us in this research area over the past four years.”
University of Adelaide Senior Research Fellow, Associate Professor Richard Young, says these findings also indicate that obese humans secrete excess serotonin from the upper gut at rest, as well as during a meal.
“This has revealed new ways that we may be able to control the release of serotonin from within the gut, and in turn, further improve the outlook for people living with obesity”, says senior co-author on the paper Associate Professor Young.
Researchers included collaborators from US pharmaceutical company Pfizer, SAHMRI, University of Adelaide Associate Professor Young and the NHMRC Centre of Research Excellence in Translating Nutritional Science to Good Health and other experts at the Flinders College of Medicine and Public Health.
The project is part of an ARC Linkage supported collaborative research project investigating the peripheral-intestinal serotonin system in humans. This system has novel and emerging roles in metabolic control, and is an exciting prospect for future novel therapies for obesity and type 2 diabetes.
Source: University of Adelaide
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract in International Journal of Obesity.
doi:10.1038/s41366-018-0047-8
[cbtabs][cbtab title=”MLA”]University of Adelaide “Obesity Trigger Identified Within Human Gut.” NeuroscienceNews. NeuroscienceNews, 22 March 2018.
<https://neurosciencenews.com/gut-trigger-obesity-8689/>.[/cbtab][cbtab title=”APA”]University of Adelaide (2018, March 22). Obesity Trigger Identified Within Human Gut. NeuroscienceNews. Retrieved March 22, 2018 from https://neurosciencenews.com/gut-trigger-obesity-8689/[/cbtab][cbtab title=”Chicago”]University of Adelaide “Obesity Trigger Identified Within Human Gut.” https://neurosciencenews.com/gut-trigger-obesity-8689/ (accessed March 22, 2018).[/cbtab][/cbtabs]
Abstract
Augmented capacity for peripheral serotonin release in human obesity
Background/objectives:
Evidence from animal studies highlights an important role for serotonin (5-HT), derived from gut enterochromaffin (EC) cells, in regulating hepatic glucose production, lipolysis and thermogenesis, and promoting obesity and dysglycemia. Evidence in humans is limited, although elevated plasma 5-HT concentrations are linked to obesity.
Subjects/methods:
We assessed (i) plasma 5-HT concentrations before and during intraduodenal glucose infusion (4 kcal/min for 30 min) in non-diabetic obese (BMI 44 ± 4 kg/m2, N = 14) and control (BMI 24 ± 1 kg/m2, N = 10) subjects, (ii) functional activation of duodenal EC cells (immunodetection of phospho-extracellular related-kinase, pERK) in response to glucose, and in separate subjects, (iii) expression of tryptophan hydroxylase-1 (TPH1) in duodenum and colon (N = 39), and (iv) 5-HT content in primary EC cells from these regions (N = 85).
Results:
Plasma 5-HT was twofold higher in obese than control responders prior to (P = 0.025), and during (iAUC, P = 0.009), intraduodenal glucose infusion, and related positively to BMI (R2 = 0.334, P = 0.003) and HbA1c (R2 = 0.508, P = 0.009). The density of EC cells in the duodenum was twofold higher at baseline in obese subjects than controls (P = 0.023), with twofold more EC cells activated by glucose infusion in the obese (EC cells co-expressing 5-HT and pERK, P = 0.001), while the 5-HT content of EC cells in duodenum and colon was similar; TPH1 expression was 1.4-fold higher in the duodenum of obese subjects (P = 0.044), and related positively to BMI (R2 = 0.310, P = 0.031).
Conclusions:
Human obesity is characterized by an increased capacity to produce and release 5-HT from the proximal small intestine, which is strongly linked to higher body mass, and glycemic control. Gut-derived 5-HT is likely to be an important driver of pathogenesis in human obesity and dysglycemia.
Note: This is an unedited manuscript that has been accepted for publication. Nature Research are providing this early version of the manuscript as a service to our customers. The manuscript will undergo copyediting, typesetting and a proof review before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers apply.






