Summary: According to researchers, people with type 2 diabetes have a higher risk of being diagnosed with Parkinson’s disease later in life. The study reports the risk may be higher for younger people and those with complications related to diabetes.
Source: AAN.
People with type 2 diabetes may have an increased risk of having a diagnosis of Parkinson’s disease later in life, according to a large study published in the June 13, 2018, online issue of Neurology. In addition, the risk may be higher for younger people and those with complications from the disease.
Parkinson’s is a progressive disease that affects a part of the brain that helps control movement. In type 2 diabetes, a person either doesn’t make enough insulin to effectively turn blood sugar into energy or the cells don’t use the insulin as well as they should.
“Our study examined data on a large portion of the English population and found a strong link between these two seemingly different diseases,” said study author Thomas T. Warner, FRCP, PhD, of University College London (UCL) in the United Kingdom. “Whether it is genetics that may play a role in the development of these diseases or they have similar pathways to development needs to be investigated further.”
For the study, researchers looked at data in a nationwide hospital database in England over 12 years and identified more than 2 million people who were admitted to the hospital for type 2 diabetes for the first time. They were then compared to more than 6 million people without diabetes who were admitted to a hospital for a range of minor medical and surgical procedures like sprains, varicose veins, appendectomy and hip replacement.
Of the more than 2 million people with diabetes, 14,252 had a diagnosis of Parkinson’s disease during a later hospital admission, compared with 20,878 of the more than 6 million people without diabetes who were later diagnosed with Parkinson’s.
After excluding conditions known to mimic Parkinson’s disease, and adjusting for age, sex, where participants lived, frequency of hospital admissions and duration of follow-up, researchers found that those with type 2 diabetes had a 31 percent greater risk of a later diagnosis of Parkinson’s disease than those without diabetes.
Researchers found the risk of being diagnosed with Parkinson’s disease later in life was even higher for younger people, ages 25 to 44. In that group, 58 of 130,728 people developed Parkinson’s, compared with 280 of 2,559,693 in the group of people without diabetes, which after adjustment amounted to a four-fold greater risk for those with diabetes. For comparison, among those who were 75 and older, there were 7,371 people out of 664,709 people with diabetes who developed Parkinson’s, compared with 10,105 out of 752,104 in the group of people without diabetes, which after adjustment amounted to an 18 percent greater risk than for those without diabetes.

In addition, those with complications from diabetes had a 49 percent greater risk of a later diagnosis of Parkinson’s disease than people without the disease, while those without diabetes complications were 30 percent more likely to develop Parkinson’s than those without the disease.
“Restoring the brain’s ability to use insulin could potentially have a protective effect on the brain,” said Warner. “It is possible that a link between type 2 diabetes and Parkinson’s could affect future diagnosis and treatment of these diseases.”
One limitation of the study was that researchers were unable to adjust results for medication and smoking. Also, because it was a hospital-based study, it is possible those diagnosed with diabetes may have had a more severe form of the disease than those who are diagnosed in a clinic.
Funding: The study was funded by the National Institute for Health Research (NIHR) Biomedical Research Centres at Oxford and University College London Hospitals in the United Kingdom.
Source: Renee Tessman – AAN
Publisher: Organized by NeuroscienceNews.com.
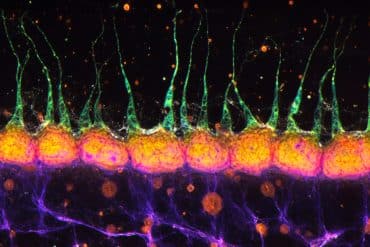
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract for “Association between diabetes and subsequent Parkinson disease: A record-linkage cohort study” by N. Eduardo De Pablo-Fernandez, Raph Goldacre, Julia Pakpoor, Alastair J. Noyce, Thomas T. Warner in Neurology. Published June 13 2018
doi:10.1212/WNL.0000000000005771
[cbtabs][cbtab title=”MLA”]AAN “Is There a Link Between Diabetes and Parkinson’s?.” NeuroscienceNews. NeuroscienceNews, 15 June 2018.
<https://neurosciencenews.com/diabetes-parkinsons-9353/>.[/cbtab][cbtab title=”APA”]AAN (2018, June 15). Is There a Link Between Diabetes and Parkinson’s?. NeuroscienceNews. Retrieved June 15, 2018 from https://neurosciencenews.com/diabetes-parkinsons-9353/[/cbtab][cbtab title=”Chicago”]AAN “Is There a Link Between Diabetes and Parkinson’s?.” https://neurosciencenews.com/diabetes-parkinsons-9353/ (accessed June 15, 2018).[/cbtab][/cbtabs]
Abstract
Association between diabetes and subsequent Parkinson disease: A record-linkage cohort study
Objective To investigate the association between type 2 diabetes mellitus (T2DM) and subsequent Parkinson disease (PD).
Methods Linked English national Hospital Episode Statistics and mortality data (1999–2011) were used to conduct a retrospective cohort study. A cohort of individuals admitted for hospital care with a coded diagnosis of T2DM was constructed, and compared to a reference cohort. Subsequent PD risk was estimated using Cox regression models. Individuals with a coded diagnosis of cerebrovascular disease, vascular parkinsonism, drug-induced parkinsonism, and normal pressure hydrocephalus were excluded from the analysis.
Results A total of 2,017,115 individuals entered the T2DM cohort and 6,173,208 entered the reference cohort. There were significantly elevated rates of PD following T2DM (hazard ratio [HR] 1.32, 95% confidence interval [CI] 1.29–1.35; p < 0.001). The relative increase was greater in those with complicated T2DM (HR 1.49, 95% CI 1.42–1.56) and when comparing younger individuals (HR 3.81, 95% CI 2.84–5.11 in age group 25–44 years).
Conclusions We report an increased rate of subsequent PD following T2DM in this large cohort study. These findings may reflect shared genetic predisposition and/or disrupted shared pathogenic pathways with potential clinical and therapeutic implications.