Summary: Researchers report harmful plaques associated with Alzheimer’s disease may build up in the brain as a result of high blood pressure and decreased cerebral blood flow.
Source: USC Dornsife.
USC researchers plan to explore whether this early sign could be targeted by drugs already approved for treating other health conditions.
A combination of high blood pressure and decreased blood flow inside the brain may spur the build-up of harmful plaque and signal the onset of dementia, USC researchers have found.
“If you have problems with the blood vessels in the brain, then you’re going to end up with difficulty with thinking skills, cognition, memory, and ultimately this can be related to other brain pathologies such as Alzheimer’s disease,” said Daniel Nation, lead author of the study and an assistant professor of psychology at USC Dornsife.
For the study published June 1 in the journal Brain, Nation used patient data from a national medical database, the Alzheimer’s Disease Neuroimaging Initiative housed at Keck School of Medicine at USC, to explore whether constricted blood flow contributes to the build-up of amyloid plaque and, consequently, to the onset of dementia. He also determined a new way to calculate cerebrovascular resistance — a stiffening of the vessels that results from high blood pressure and low blood flow.
The brain’s blood vessels function as a plumbing system that delivers nutrients and oxygen to feed the brain cells, and then flushes away any waste that the cells cannot use. The metabolic waste secreted by cells includes protein fragments — called amyloid — that a healthy brain breaks down and expels by pulsating blood through its vessels.
The brain tightens or relaxes its vessels to maintain blood flow as it adjusts for changes in blood pressure. However, the brain vessels in Alzheimer’s patients are stiff and tight, inhibiting blood flow and enabling the sticky amyloid to accumulate, Nation found.
“The idea of cerebrovascular resistance converges on the notion that the blood vessels in Alzheimer’s brains are in this hyper-contracted state,” Nation said. “For many different reasons, the contracting blood vessels are resistant to opening up and really letting the blood in.”
Blood pressure and blood flow measures alone do not predict dementia as well as when they are examined together.
“When blood pressure goes up or down, the brain vessels accommodate so that blood flow will remain fixed,” Nation said. “So if you don’t measure blood pressure and blood flow together, then it is basically masking all of these important changes in vascular resistance, and it is very difficult to see the vessel changes that underlie this.”
Dementia and Alzheimer’s: A rising health crisis
Alzheimer’s is considered one of the greatest health challenges of the century. Alzheimer’s affects an estimated 5.4 million Americans — about 1 in 3 seniors. As a research institution devoted to promoting lifelong health, USC researchers across a range of disciplines are examining the health, societal and political effects and implications of the disease.
Nation’s lab at USC Dornsife is part of the multidisciplinary effort. He focuses on understanding cognitive decline associated with age-related changes in vascular structure and function.
High resistance in Alzheimer’s patients
To measure resistance in the brain’s vessels, Nation developed an index that represents a ratio of average blood pressure to regional cerebral blood flow. A high index ranking for resistance indicates that amyloid is building up and that the patient is progressing toward dementia, Nation said.
The Alzheimer’s Disease Neuroimaging Initiative database used for the study is an extensive repository of medical data from an estimated 1,000 volunteers age 55–90. The data include results of genetic, memory and cognitive tests, brain scans and blood biomarker information.
Nation used data on three groups of volunteer men and women: those who did not have any amyloid buildup in their brains, those who did, and those who had Alzheimer’s disease.
Nation found that the people with Alzheimer’s disease had lower blood flow in their brains than the people without dementia. These blood flow changes were undetectable in the earlier stages of disease, when amyloid was accumulating but there were no obvious signs of memory loss.
The people with Alzheimer’s disease also measured much higher on the cerebrovascular resistance index.
Amyloid-positive patients’ cognition worsened over time. Nation found that just two years after their initial examination, they were more likely to experience accelerated cognitive decline and progression to clinical dementia.
“Our findings suggest that change in resistance may be an early and key phenomenon in the brain that’s closely linked to the symptoms of cognitive decline in the future,” Nation said.
Potential dementia blockers
In recent months, major pharmaceutical companies aiming for a cure have halted testing of Alzheimer’s drugs mid-trial due to poor results. However, recent studies point to a promising option to delay the onset of dementia or Alzheimer’s: drugs already on the market and approved by the U.S. Food and Drug Administration for other purposes.
Among the most promising are cholesterol-lowering statins and blood pressure-lowering drugs known as angiotensin receptor blockers. The latter were highlighted by Nation in a recent study published in Alzheimer’s Research & Therapy.
He found that people taking blood pressure-lowering drugs have better memories than people who have elevated blood pressure and are taking other drugs. A subclass of these drugs can cross the blood-brain barrier — the filtration mechanism in the capillaries that prevents toxins from entering the brain.
Nation said he aims to refine how he measures vascular resistance so that he can test it in older adults in the lab. By measuring the index dynamically with brain scanners, he will track how blood pressure-lowering drugs affect vascular resistance from moment to moment in the brains of people at risk of Alzheimer’s disease.
Then, he will work toward answering the next important question: If vascular resistance can be managed with treatments, will that lower someone’s risk for developing dementia?
USC graduate student Belinda Yew was a co-author of the cerebrovascular resistance study published in Brain, and USC graduate student Jean Ho was a co-author on the blood-pressure-lowering drugs study published in Alzheimer’s Research & Therapy. The research was supported by National Institutes of Health grants P50 AG005142 (an estimated $7.1 million grant that covered 10 percent of the study’s costs) and P01 AG052350 (an estimated $8.9 million grant that covered 20 percent of the study’s costs). The NIH grants also support a series of studies by Nation.
The remaining 70 percent of the Brain study’s costs were covered by the Alzheimer’s Disease Neuroimaging Initiative and a U.S. Department of Defense grant (W81XWH-12-2-0012).
Source: Michelle Boston and Emily Gersema – USC Dornsife
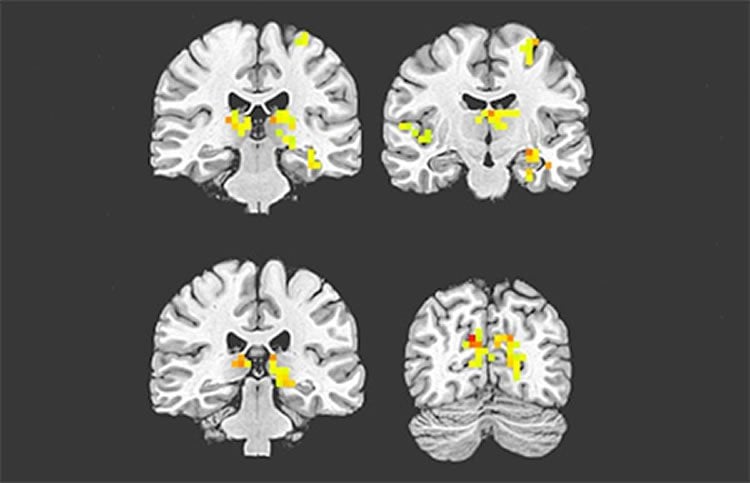
Image Source: NeuroscienceNews.com image is credited to Daniel Nation.
Original Research: Abstract for “Cerebrovascular resistance: effects on cognitive decline, cortical atrophy, and progression to dementia” by Belinda Yew, Daniel A. Nation, for the Alzheimer’s Disease Neuroimaging Initiative in Brain. Published online June 1 2017 doi:10.1093/brain/awx112
[cbtabs][cbtab title=”MLA”]USC Dornsife “Stiff Vessels and Low Blood Flow in the Brain Forewarn of Dementia.” NeuroscienceNews. NeuroscienceNews, 28 June 2017.
<https://neurosciencenews.com/dementia-stiff-vessel-blood-flow-7015/>.[/cbtab][cbtab title=”APA”]USC Dornsife (2017, June 28). Stiff Vessels and Low Blood Flow in the Brain Forewarn of Dementia. NeuroscienceNew. Retrieved June 28, 2017 from https://neurosciencenews.com/dementia-stiff-vessel-blood-flow-7015/[/cbtab][cbtab title=”Chicago”]USC Dornsife “Stiff Vessels and Low Blood Flow in the Brain Forewarn of Dementia.” https://neurosciencenews.com/dementia-stiff-vessel-blood-flow-7015/ (accessed June 28, 2017).[/cbtab][/cbtabs]
Abstract
Cerebrovascular resistance: effects on cognitive decline, cortical atrophy, and progression to dementia
Evidence for vascular contributions to Alzheimer’s disease has been increasingly identified, with increased blood pressure and decreased cerebral blood flow both linked to in vivo biomarkers and clinical progression of Alzheimer’s disease. We therefore hypothesized that an elevated ratio of blood pressure to cerebral blood flow, indicative of cerebrovascular resistance, would exhibit earlier and more widespread associations with Alzheimer’s disease than cerebral blood flow alone. Further, we predicted that increased cerebrovascular resistance and amyloid retention would synergistically influence cognitive performance trajectories, independent of neuronal metabolism. Lastly, we anticipated associations between cerebrovascular resistance and later brain atrophy, prior to amyloid accumulation. To evaluate these hypotheses, we investigated associations between cerebrovascular resistance and amyloid retention, cognitive decline, and brain atrophy, controlling for neuronal metabolism. North American older adults (n = 232) underwent arterial spin labelling magnetic resonance imaging to measure regional cerebral blood flow in brain regions susceptible to ageing and Alzheimer’s disease. An estimated cerebrovascular resistance index was then calculated as the ratio of mean arterial pressure to regional cerebral blood flow. Positron emission tomography with 18F-florbetapir and fludeoxyglucose was used to quantify amyloid retention and neuronal metabolism, respectively. Cognitive performance was evaluated via annual assessments of global cognition, memory, and executive function. Results indicated diminished inferior parietal and temporal cerebral blood flow for patients with Alzheimer’s disease (n = 33) relative to both non-demented groups, but no cerebral blood flow differences between non-demented amyloid-positive (n = 87) and amyloid-negative (n = 112) cases. In contrast, the cerebrovascular resistance index was significantly elevated in amyloid-positive versus amyloid-negative cases, with additional elevation in patients with Alzheimer’s disease. Furthermore, cerebrovascular resistance index group differences were of greater statistical effect size and encompassed a greater number of brain regions than those for cerebral blood flow alone. Cognitive decline over 2-year follow-up was accelerated by elevated baseline cerebrovascular resistance index, particularly for amyloid-positive individuals. Increased baseline cerebrovascular resistance index also predicted greater progression to dementia, beyond that attributable to amyloid-positivity. Finally, increased cerebrovascular resistance index predicted greater regional atrophy among non-demented older adults who were amyloid-negative. Findings suggest that increased cerebrovascular resistance may represent a previously unrecognized contributor to Alzheimer’s disease that is independent of neuronal hypometabolism, predates changes in brain perfusion, exacerbates and works synergistically with amyloidosis to produce cognitive decline, and drives amyloid-independent brain atrophy during the earliest stage of disease.
“Cerebrovascular resistance: effects on cognitive decline, cortical atrophy, and progression to dementia” by Belinda Yew, Daniel A. Nation, for the Alzheimer’s Disease Neuroimaging Initiative in Brain. Published online June 1 2017 doi:10.1093/brain/awx112






