BWH researchers find evidence that diet and gut microbes can remotely influence brain inflammation.
New research by investigators at Brigham and Women’s Hospital (BWH) suggests that bacteria living in the gut may remotely influence the activity of cells in the brain that are involved in controlling inflammation and neurodegeneration. Using pre-clinical models for multiple sclerosis (MS) and samples from MS patients, the team found evidence that changes in diet and gut flora may influence astrocytes in the brain, and, consequently, neurodegeneration, pointing to potential therapeutic targets. The team’s results are published this week in Nature Medicine.
“For the first time, we’ve been able to identify that food has some sort of remote control over central nervous system inflammation,” said corresponding author Francisco Quintana, PhD, an investigator in the Ann Romney Center for Neurologic Diseases at BWH. “What we eat influences the ability of bacteria in our gut to produce small molecules, some of which are capable of traveling all the way to the brain. This opens up an area that’s largely been unknown until now: how the gut controls brain inflammation.”
Previous investigations have suggested a connection between the gut microbiome and brain inflammation, but how the two are linked and how diet and microbial products influence this connection has remained largely unknown. To explore this connection further, Quintana and colleagues performed genome-wide transcriptional analyses on astrocytes — star-shaped cells that reside in the brain and spinal cord – in a mouse model of MS, identifying a molecular pathway involved in inflammation. They found that molecules derived from dietary tryptophan (an amino acid famously found in turkey and other foods) act on this pathway, and that when more of these molecules are present, astrocytes were able to limit brain inflammation. In blood samples from MS patients, the team found decreased levels of these tryptophan-derived molecules.
“Deficits in the gut flora, deficits in the diet or deficits in the ability to uptake these products from the gut flora or transport them from the gut — any of these may lead to deficits that contribute to disease progression,” said Quintana.
The research team plans to investigate this pathway and the role of diet in future studies to determine if the new findings can be translated into targets for therapeutic intervention and biomarkers for diagnosing and detecting the advancement of disease.
Funding: This work was supported by grants from the National Institutes of Health, the National Multiple Sclerosis Society, Mallinkrodt Pharmaceuticals, the German Research Foundation, the International Academy of Life Sciences, the Ministry of Science and Technology, Taiwan, and by a fellowship CAPES, Brazil.
Source: Haley Bridger – Brigham and Women’s Hospital
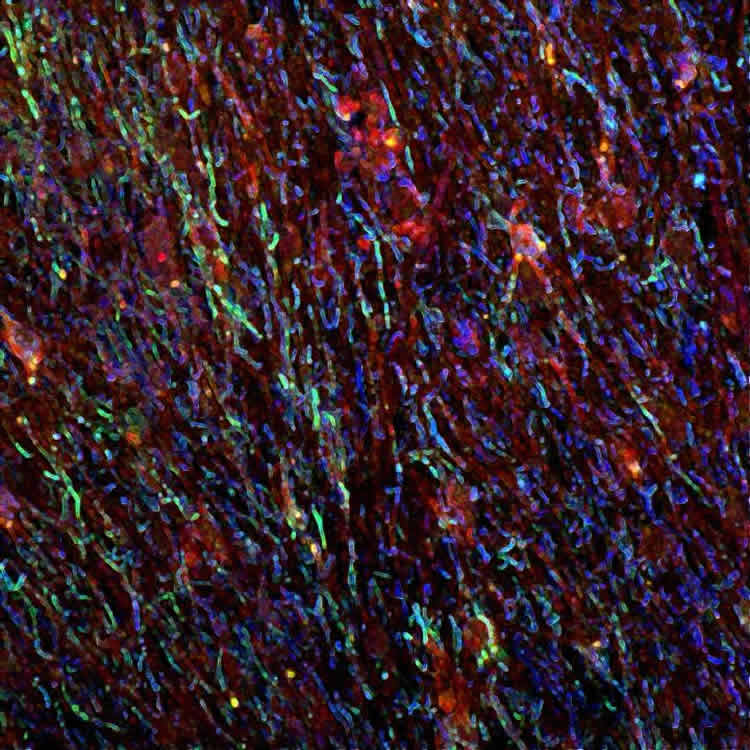
Image Source: The image is credited to Jorge Ivan Alvarez, Assistant Professor at the Department of Pathobiology, School of Veterinary Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Original Research: Abstract for “Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor” by Veit Rothhammer, Ivan D Mascanfroni, Lukas Bunse, Maisa C Takenaka, Jessica E Kenison, Lior Mayo, Chun-Cheih Chao, Bonny Patel, Raymond Yan, Manon Blain, Jorge I Alvarez, Hania Kébir, Niroshana Anandasabapathy, Guillermo Izquierdo, Steffen Jung, Nikolaus Obholzer, Nathalie Pochet, Clary B Clish, Marco Prinz, Alexandre Prat, Jack Antel and Francisco J Quintana in Nature Medicine. Published online May 9 2016 doi:10.1038/nm.4106
Abstract
Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor
Astrocytes have important roles in the central nervous system (CNS) during health and disease. Through genome-wide analyses we detected a transcriptional response to type I interferons (IFN-Is) in astrocytes during experimental CNS autoimmunity and also in CNS lesions from patients with multiple sclerosis (MS). IFN-I signaling in astrocytes reduces inflammation and experimental autoimmune encephalomyelitis (EAE) disease scores via the ligand-activated transcription factor aryl hydrocarbon receptor (AHR) and the suppressor of cytokine signaling 2 (SOCS2). The anti-inflammatory effects of nasally administered interferon (IFN)-β are partly mediated by AHR. Dietary tryptophan is metabolized by the gut microbiota into AHR agonists that have an effect on astrocytes to limit CNS inflammation. EAE scores were increased following ampicillin treatment during the recovery phase, and CNS inflammation was reduced in antibiotic-treated mice by supplementation with the tryptophan metabolites indole, indoxyl-3-sulfate, indole-3-propionic acid and indole-3-aldehyde, or the bacterial enzyme tryptophanase. In individuals with MS, the circulating levels of AHR agonists were decreased. These findings suggest that IFN-Is produced in the CNS function in combination with metabolites derived from dietary tryptophan by the gut flora to activate AHR signaling in astrocytes and suppress CNS inflammation.
“Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor” by Veit Rothhammer, Ivan D Mascanfroni, Lukas Bunse, Maisa C Takenaka, Jessica E Kenison, Lior Mayo, Chun-Cheih Chao, Bonny Patel, Raymond Yan, Manon Blain, Jorge I Alvarez, Hania Kébir, Niroshana Anandasabapathy, Guillermo Izquierdo, Steffen Jung, Nikolaus Obholzer, Nathalie Pochet, Clary B Clish, Marco Prinz, Alexandre Prat, Jack Antel and Francisco J Quintana in Nature Medicine. Published online May 9 2016 doi:10.1038/nm.4106






