Summary: A new study finds that older adults with gum disease are more likely to show signs of white matter damage in the brain — a change tied to memory decline, balance issues, and higher stroke risk. MRI scans revealed that participants with gum disease had significantly more white matter hyperintensities than those without, even after accounting for age and other health factors.
Researchers emphasize that while the study doesn’t prove causation, it highlights a potential link between oral inflammation and brain health. The findings suggest that maintaining good dental hygiene may also help protect the brain as we age.
Key Facts:
- White Matter Damage: Adults with gum disease had more white matter hyperintensities — signs of nerve fiber damage in the brain.
- 56% Higher Odds: Participants with gum disease were 56% more likely to show severe white matter changes than those without.
- Brain–Mouth Connection: Findings suggest oral inflammation may contribute to cerebral small vessel disease and cognitive decline.
Source: AAN
Adults with gum disease may be more likely to have signs of damage to the brain’s white matter, called white matter hyperintensities, than people without gum disease, according to a new study published on October 22, 2025, in Neurology Open Access.
White matter refers to nerve fibers that help different parts of the brain communicate. Damage to this tissue can affect memory, thinking, balance and coordination and has been linked to higher stroke risk.
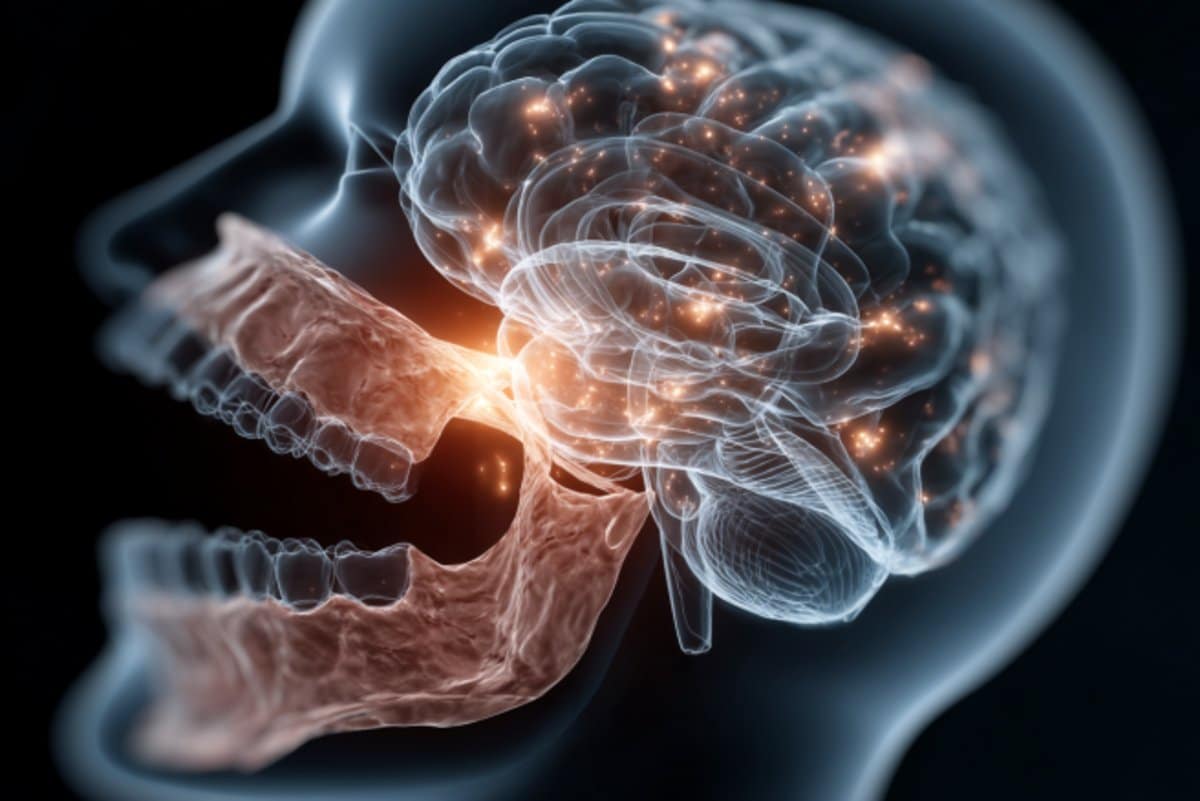
White matter hyperintensities are bright spots that appear on brain scans that are thought to reflect damaged white matter tissue. While the study found an association, it does not prove that gum disease causes white matter damage.
“This study shows a link between gum disease and white matter hyperintensities suggesting oral health may play a role in brain health that we are only beginning to understand,” said study author Souvik Sen, MD, MS, MPH, of the University of South Carolina in Columbia.
“While more research is needed to understand this relationship, these findings add to growing evidence that keeping your mouth healthy may support a healthier brain.”
The study included 1,143 adults with an average age of 77. Each person had a dental exam to check for gum disease. Of participants, 800 had gum disease and 343 did not.
Participants had brain scans to look for signs of cerebral small vessel disease, which is damage in the brain’s small blood vessels that can appear as white matter hyperintensities, cerebral microbleeds or lacunar infarcts.
These brain changes become more common with age and are associated with increased risk of stroke, memory problems and mobility issues.
People with gum disease had more white matter hyperintensities, with an average volume of 2.83% of total brain volume compared to 2.52% for people without gum disease.
Researchers divided people into four groups based on white matter hyperintensity volume. Those in the highest group had a volume of more than 21.36 centimeters cubed (cm³) while those in the lowest group had a volume of less than 6.41 cm³.
Of people with gum disease, 28% were in the highest group compared to 19% of people without gum disease.
After adjusting for factors such as age, sex, race, high blood pressure, diabetes and smoking, people with gum disease had 56% higher odds of falling into the highest group of white matter hyperintensities than people without gum disease.
However, no links were found between gum disease and two other brain changes tied to small vessel disease, cerebral microbleeds and lacunar infarcts.
“Gum disease is preventable and treatable,” said Sen.
“If future studies confirm this link, it could offer a new avenue for reducing cerebral small vessel disease by targeting oral inflammation. For now, it underscores how dental care may support long-term brain health.”
A limitation of the study is that brain imaging and dental assessments were conducted only once, making it difficult to assess changes over time.
Key Questions Answered:
A: Researchers found that people with gum disease had significantly more white matter hyperintensities — small areas of brain damage linked to aging, stroke, and memory loss — suggesting oral inflammation may influence brain health.
A: White matter hyperintensities are bright spots on MRI scans that indicate damaged nerve fibers. They are associated with cognitive decline, balance problems, and higher risk of stroke.
A: While this study only shows an association, not causation, experts say maintaining oral health may reduce systemic inflammation and potentially support better brain function over time.
About this neurology research news
Author: Natalie Conrad
Source: AAN
Contact: Natalie Conrad – AAN
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Periodontal Disease Independently Associated With White Matter Hyperintensity Volume: A Measure of Cerebral Small Vessel Disease” by Souvik Sen et al. Neurology: Open Access
Abstract
Periodontal Disease Independently Associated With White Matter Hyperintensity Volume: A Measure of Cerebral Small Vessel Disease
Background and Objectives
White matter hyperintensities (WMHs), cerebral microbleeds (CMBs), and lacunar infarcts are radiographic markers of cerebral small vessel disease (CSVD), which is associated with an increased risk of stroke and cognitive decline. Periodontal disease (PD), a chronic inflammatory condition, has been linked to vascular pathology and may contribute to CSVD. The aim of this study was to assess the independent association between PD and MRI-verified CSVD features using data from the Atherosclerosis Risk in Communities (ARIC) cohort.
Methods
Periodontal status was classified as PD (n = 800) or periodontal health ([PH]; n = 343). CSVD features included WMH volume (WMHV), CMBs, and lacunar infarcts. WMHV was derived from fluid-attenuated inversion recovery images and categorized into quartiles. Multinomial logistic regression was used to evaluate associations between PD and WMHV quartiles, and binomial logistic regression assessed associations between PD and the presence of CMBs and lacunar infarcts. Models were adjusted for demographic and vascular risk factors including age, sex, race-center, hypertension, diabetes, smoking status, and time between visits.
Results
We analyzed 1,143 ARIC participants (mean age 77 years; 45% male; 76% White, 24% African American) who underwent periodontal assessment at Visit 4 and brain MRI at Visit 5. Participants with PD had significantly greater WMHV compared with those with PH (median WMH%: 2.83 vs 2.52; p = 0.012). PD was associated with the highest WMHV quartile (Q4 >21.36 cm3), with a crude odds ratio (OR) of 1.77 (95% CI 1.23–2.56) and an adjusted OR of 1.56 (95% CI 1.01–2.40). A weak but significant correlation was found between WMHV and World Workshop Periodontal Profile Class (ρ = 0.076, p = 0.011). No statistically significant adjusted associations were found between PD and CMBs (adj. OR 1.16, 95% CI 0.83–1.63) or lacunar infarcts (adj. OR 1.14, 95% CI 0.77–1.69).
Discussion
PD was independently associated with greater WMH burden, a key imaging marker of CSVD, but not with CMBs or lacunar infarcts after adjustment for confounders. This suggests that PD may contribute to CSVD pathology, particularly WMHs, through mechanisms involving systemic inflammation. Limitations include the temporal gap between dental and imaging assessments and potential residual confounding. Interventions targeting PD could be explored as a modifiable risk factor for CSVD prevention.






