Vitamin D insufficiency among the elderly is highly correlated with accelerated cognitive decline and impaired performance, particularly in domains such as memory loss that are associated with Alzheimer’s disease and dementia, researchers with the UC Davis Alzheimer’s Disease Center and Rutgers University have found. The effect is “substantial,” with individuals with low vitamin D declining at a rate three times faster than those with adequate vitamin D levels.
The researchers said their findings amplify the importance of identifying vitamin D insufficiency among the elderly, particularly high-risk groups such as African-Americans and Hispanics, who are less able to absorb the nutrient from its most plentiful source: sunshine. Among those groups and other darker-skinned individuals, low vitamin D should be considered a risk factor for dementia, they said.
The research is published online today in JAMA Neurology, a JAMA Network journal.
“Independent of race or ethnicity, baseline cognitive abilities and a host of other risk factors, vitamin D insufficiency was associated with significantly faster declines in both episodic memory and executive function performance,” said Joshua Miller, professor in the Department of Pathology and Laboratory Medicine at the time when the research was conducted and now professor and chair of the Department of Nutritional Sciences at Rutgers University.
“This work, and that of others, suggests that there is enough evidence to recommend that people in their 60s and older discuss taking a daily vitamin D supplement with their physicians,” Miller said.
“Even if doing so proves to not be effective, there’s still very low health risk to doing it,” he said.
The large, longitudinal study was conducted in nearly 400 racially and ethnically diverse men and women in Northern California participating in longitudinal research at the Alzheimer’s Disease Center in Sacramento, Calif. Fifty percent of participants were Caucasian and 50 percent were African-American or Hispanic. The participants had a mean age of 76 and were either cognitively normal, had mild cognitive impairment, or dementia.
The participants’ serum vitamin D status was measured at the beginning of the study. Vitamin D deficiency and insufficiency were prevalent among all of the study participants. Overall, 26 percent were deficient and 35 percent were insufficient. Among Caucasians, 54 percent had low vitamin D, compared with 70 percent of African-Americans and Hispanics.
Over five years of follow-up, vitamin D deficient individuals experienced cognitive declines that were two-to-three times faster than those with adequate serum vitamin D levels. In other words it took only two years for the deficient individuals to decline as much as their counterparts with adequate Vitamin D declined during the five-year follow-up period.
“We expected to see declines in individuals with low vitamin D status,” said Charles DeCarli, director of the Alzheimer’s Disease Center. “What was unexpected was how profoundly and rapidly [low vitamin D] impacts cognition.”
Exposing the skin to sunlight is the major source of vitamin D. Racial and some ethnic minorities are at greater risk of low vitamin D because the higher concentration of melanin that makes their skin darker — and protects against skin cancer in sunny climates — also inhibits synthesis of vitamin D.
Diet is the other major source of vitamin D. Dietary vitamin D is obtained particularly through dairy consumption. The intake of dairy products is especially low among minority groups, with only 6.5 percent of African-Americans and 11 percent of Mexican-Americans nationwide consuming the recommended three daily servings of dairy products, the study says.
“I don’t know if replacement therapy would affect these cognitive trajectories. That needs to be researched and we are planning on doing that,” DeCarli said.
“This is a vitamin deficiency that could easily be treated and that has other health consequences. We need to start talking about it. And we need to start talking about it, particularly for people of color, for whom vitamin D deficiency appears to present an even greater risk,” he said.
Other study authors include Danielle J. Harvey, Laurel Beckett, Ralph Green, Sarah Farias, Bruce Reed, John Olichney and Dan Mungas, all of UC Davis.
Funding: The study was funded by a grant from the National Institutes of Health P30 AG010129 to DeCarli.
Source: Phyllis Brown – UC Davis
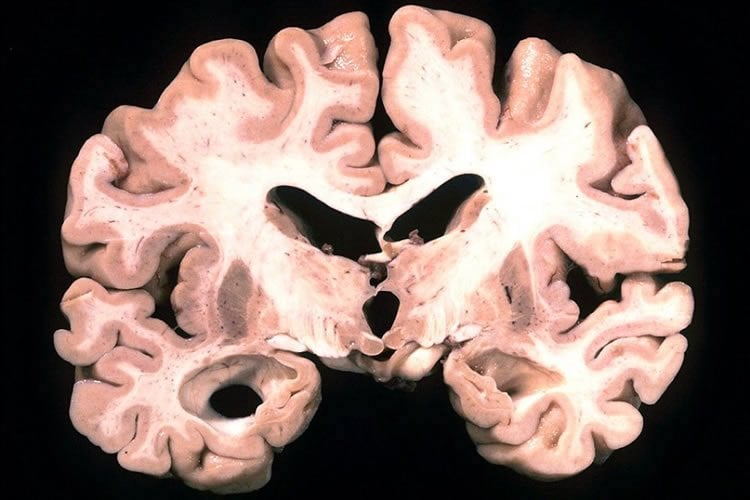
Image Credit: The image is in the public domain
Original Research: Full open access research for “Vitamin D Status and Rates of Cognitive Decline in a Multiethnic Cohort of Older Adults” by Joshua W. Miller, PhD; Danielle J. Harvey, PhD; Laurel A. Beckett, PhD; Ralph Green, MD, PhD; Sarah Tomaszewski Farias, PhD; Bruce R. Reed, PhD; John M. Olichney, MD; Dan M. Mungas, PhD; and Charles DeCarli, MD in JAMA Neurology. Published online September 14 2015 doi:10.1001/jamaneurol.2015.2115
Abstract
Vitamin D Status and Rates of Cognitive Decline in a Multiethnic Cohort of Older Adults
Importance Vitamin D (VitD) deficiency is associated with brain structural abnormalities, cognitive decline, and incident dementia.
Objective To assess associations between VitD status and trajectories of change in subdomains of cognitive function in a cohort of ethnically diverse older adults.
Design, Setting, and Participants Longitudinal multiethnic cohort study of 382 participants in an outpatient clinic enrolled between February 2002 and August 2010 with baseline assessment and yearly follow-up visits. Serum 25-hydroxyvitamin D (25-OHD) was measured, with VitD status defined as the following: deficient, less than 12 ng/mL (to convert to nanomoles per liter, multiply by 2.496); insufficient, 12 to less than 20 ng/mL; adequate, 20 to less than 50 ng/mL; or high, 50 ng/mL or higher. Subdomains of cognitive function were assessed using the Spanish and English Neuropsychological Assessment Scales. Associations were evaluated between 25-OHD levels (as continuous and categorical [deficient, insufficient, or adequate]) and trajectories of cognitive decline.
Main Outcomes and Measures Serum 25-OHD levels, cognitive function, and associations between 25-OHD levels and trajectories of cognitive decline.
Results Participants (N = 382 at baseline) had a mean (SD) age of 75.5 (7.0) years; 61.8% were women; and 41.4% were white, 29.6% African American, 25.1% Hispanic, and 3.9% other race/ethnicity. Diagnosis at enrollment included 17.5% with dementia, 32.7% with mild cognitive impairment, and 49.5% cognitively normal. The mean (SD) 25-OHD level was 19.2 (11.7) ng/mL, with 26.2% of participants being VitD deficient and 35.1% insufficient. The mean (SD) 25-OHD levels were significantly lower for African American and Hispanic participants compared with white participants (17.9 [15.8] and 17.2 [8.4] vs 21.7 [10.0] ng/mL, respectively; P < .001 for both). The mean (SD) 25-OHD levels were similarly lower in the dementia group compared with the mild cognitive impairment and cognitively normal groups (16.2 [9.4] vs 20.0 [10.3] and 19.7 [13.1] ng/mL, respectively; P = .006). The mean (SD) follow-up was 4.8 (2.5) years. Rates of decline in episodic memory and executive function among VitD-deficient (episodic memory: β = −0.04 [SE = 0.02], P = .049; executive function: β = −0.05 [SE = 0.02], P = .01) and VitD-insufficient (episodic memory: β = −0.06 [SE = 0.02], P < .001; executive function: β = −0.04 [SE = 0.02], P = .008) participants were greater than those with adequate status after controlling for age, sex, education, ethnicity, body mass index, season of blood draw, vascular risk, and apolipoprotein E4 genotype. Vitamin D status was not significantly associated with decline in semantic memory or visuospatial ability. Exclusion of participants with dementia did not substantially affect the associations between VitD status and rates of cognitive decline.
Conclusions and Relevance Low VitD status was associated with accelerated decline in cognitive function domains in ethnically diverse older adults, including African American and Hispanic individuals who exhibited a high prevalence of VitD insufficiency or deficiency. It remains to be determined whether VitD supplementation slows cognitive decline.
“Vitamin D Status and Rates of Cognitive Decline in a Multiethnic Cohort of Older Adults” by Joshua W. Miller, PhD; Danielle J. Harvey, PhD; Laurel A. Beckett, PhD; Ralph Green, MD, PhD; Sarah Tomaszewski Farias, PhD; Bruce R. Reed, PhD; John M. Olichney, MD; Dan M. Mungas, PhD; and Charles DeCarli, MD in JAMA Neurology. Published online September 14 2015 doi:10.1001/jamaneurol.2015.2115







