Summary: Disrupting circadian rhythms during adolescence may alter how the brain responds to prenatal infections, a known risk factor for disorders like schizophrenia and autism. In a new mouse study, researchers found that each factor alone changed behavior and brain activity, but their combination produced unique effects—sometimes even counteracting one another.
The findings suggest that risk factors for brain disorders may interact in surprising ways, with circadian disruption not always making outcomes worse. Adolescence appears to be a particularly vulnerable period, making regular sleep-wake cycles crucial for brain development.
Key Facts:
- Dual Risk Interaction: Prenatal infection and adolescent circadian disruption together altered behavior and gene activity more than either alone.
- Unexpected Moderation: Circadian disruption sometimes reduced the negative effects of prenatal infection.
- Adolescent Vulnerability: Teen sleep patterns and light exposure may influence long-term brain health.
Source: McGill University
A new McGill University-led study suggests that disrupting the body’s internal clock during adolescence can alter how the brain responds to an in-utero risk factor linked to certain brain disorders.
Previous research has shown that a mother’s infection during pregnancy, such as the flu, can increase a child’s risk of developing conditions like schizophrenia and autism spectrum disorders later in life. Irregular sleep patterns – often a sign of circadian rhythm disruption – are also associated with these conditions.

To investigate how these factors interact, researchers exposed mice to either a prenatal infection, circadian disruption during adolescence (via constant light exposure), both or neither.
They found that each factor caused some changes on its own, but the combination altered memory, anxiety, social behaviour and gene activity in brain regions associated with the disorders.
“While more research is needed, our findings suggest that people exposed to multiple risk factors may need to be especially mindful of their daily rhythms,” said lead author Tara Delorme, who conducted the research as a PhD student at the Douglas Research Centre.
Surprisingly, the combined effects didn’t always make outcomes worse.
“We assumed the effects would be additive,” said senior author Nicolas Cermakian, a professor in McGill’s Department of Psychiatry.
“But in some cases, disruption of biological rhythms actually reduced the impact of prenatal infection. That suggests these factors may interact in unexpected ways.”
The researchers focused on adolescence because it’s a sensitive period for brain development.
“Adolescents are vulnerable,” said Cermakian. “Their internal clocks tend to run later than the rest of the population, but school still starts early. On top of that, evening exposure to screens and artificial light can further delay their biological rhythms, leading to what we call social jet lag.”
This mismatch between the body’s internal clock and daily schedules has been linked to a range of health issues, he added.
The research team, including McGill psychiatry professors and Douglas researchers Lalit Srivastava and Patricia Silveira, is now investigating the gene changes the researchers saw in mice to see what they might reveal about how the human brain develops.
Funding:
The research was supported by the Canadian Institutes of Health Research, Velux Stiftung, the Fonds de recherche du Québec, the Ludmer Centre for Neuroinformatics and Mental Health and the McGill Interdisciplinary Initiative in Infection and Immunity.
About this neurodevelopment research news
Author: Keila DePape
Source: McGill University
Contact: Keila DePape – McGill University
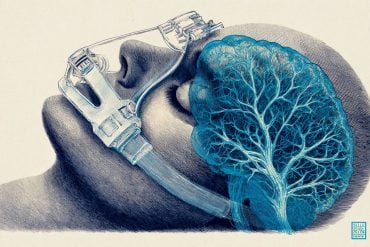
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Large-scale effects of prenatal inflammation and early life circadian disruption in mice: Implications for neurodevelopmental disorders” by Tara Delorme et al. Brain, Behavior, and Immunity
Abstract
Large-scale effects of prenatal inflammation and early life circadian disruption in mice: Implications for neurodevelopmental disorders
Around 80 % of individuals with neurodevelopmental disorders such as schizophrenia and autism spectrum disorders experience disruptions in sleep/circadian rhythms.
We explored whether environmental circadian disruption interacts with prenatal infection, a risk factor for neurodevelopmental disorders, to induce sex-specific deficits in mice.
A maternal immune activation (MIA) protocol was used by injecting pregnant mice with viral mimic poly IC or saline at E9.5.
Juvenile/adolescent male and female offspring (3–7 weeks old) were then subjected to a standard light:dark cycle (12:12LD) or to constant light (LL).
Significant interactions between treatment (MIA, control) and lighting (12:12LD, LL) were evident in behaviors related to cognition, anxiety, and sociability.
This pattern persisted in our RNA sequencing analysis of the dorsal hippocampus, where poly IC exposure resulted in numerous differentially expressed genes (DEGs) in males, while exposure to both poly IC and LL led to a marked reduction in DEGs.
Through WGCNA analysis, many significant gene modules were found to be positively associated with poly IC (vs. saline) and LL (vs. LD) in males (fewer in females).
Many of the identified hub-bottleneck genes were homologous to human genes associated with sleep/circadian rhythms and neurodevelopmental disorders as revealed by GWA studies.
The MIA- and LL-associated modules were enriched in microglia gene signatures, which was paralleled by trends of effects of each of the factors on microglia morphology.
In conclusion, in a mouse model of prenatal infection, circadian disruption induced by LL during adolescence acts as a modulator of the effects of MIA at behavioral, cellular, and molecular levels.