Summary: Rats susceptible to anhedonia have more serotonin neurons in the ventral dorsal raphe nucleus. However, activating neurons in the central amygdala reduced the serotonin signaling and lowered the effects of social stress.
Source: SfN
Rats susceptible to anhedonia, a core symptom of depression, possess more serotonin neurons after being exposed to chronic stress, but the effect can be reversed through amygdala activation, according to new research in Journal of Neuroscience.
Some people are resistant to depression and anhedonia, or lack of pleasure, even when exposed to chronic stress. To measure susceptibility to anhedonia, Prakash et al. trained rats to activate an electrode that stimulated reward circuits in their brain, causing feelings of pleasure. The rats experienced social stress once a day and then were given access to self-stimulation fifteen minutes later. In rats susceptible to anhedonia, the stress dramatically increased the intensity of stimulation needed to feel pleasure, while it had little effect on the resilient rats.
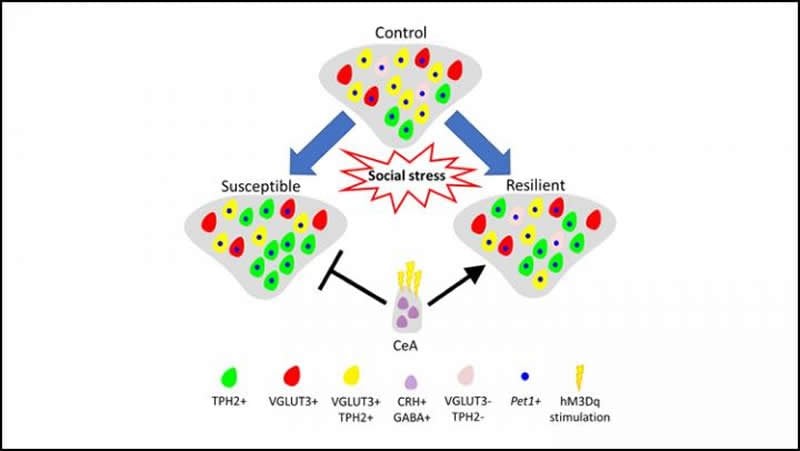
Compared to the resilient rats, the susceptible rats had more serotonin neurons in the ventral part of their dorsal raphe nucleus, an area of the brain involved in regulating stress and reward. This increase is due to the recruitment of non-serotonin signaling neurons. When the researchers activated neurons in the central amygdala to prevent the increase in serotonin signaling, the rats experienced reduced effects from social stress.
Understanding the molecular thumbprint of depression susceptibility could lead to treatments that induce resilience in the face of chronic stress.
Funding: This work was supported by the following grants: the Kavli Institute for Brain and Mind (Grant No. 2012-008 [to DD]), the Tobacco-Related Disease Research Program (Grant No. 27IR-0020 [to DD]), the National Institute of Drug Addiction (Grant No. R21-DA047455 [to DD]), the National Institute of Mental Health (Grant No. R01 MH106865 [to AD]), and the National Institute on Alcohol Abuse and Alcoholism (Grant No. R01 AA026560 [to AD]).
Source:
SfN
Media Contacts:
Calli McMurray – SfN
Image Source:
The image is credited to Prakash et al., JNeurosci 2019.
Original Research: Closed access
“Serotonergic Plasticity in the Dorsal Raphe Nucleus Characterizes Susceptibility and Resilience to Anhedonia”. Nandkishore Prakash, Christiana J. Stark, Maria N. Keisler, Lily Luo, Andre Der-Avakian and Davide Dulcis.
Journal of Neuroscience doi:10.1523/JNEUROSCI.1802-19.2019.
Abstract
Serotonergic Plasticity in the Dorsal Raphe Nucleus Characterizes Susceptibility and Resilience to Anhedonia
Chronic stress induces anhedonia in susceptible but not resilient individuals, a phenomenon observed in humans as well as animal models, but the molecular mechanisms underlying susceptibility and resilience are not well understood. We hypothesized that the serotonergic system, which is implicated in stress, reward and antidepressant therapy, may play a role. We found that plasticity of the serotonergic system contributes to the differential vulnerability to stress displayed by susceptible and resilient animals. Stress-induced anhedonia was assessed in adult male rats using social defeat and intracranial self-stimulation (ICSS), while changes in serotonergic phenotype were investigated using immunohistochemistry and in situ hybridization. Susceptible, but not resilient, rats displayed an increased number of neurons expressing the biosynthetic enzyme for serotonin, tryptophan-hydroxylase-2 (TPH2), in the ventral subnucleus of the dorsal raphe nucleus (DRv). Further, a decrease in the number of DRv glutamatergic (VGLUT3+) neurons was observed in all stressed rats. This neurotransmitter plasticity is activity-dependent, as was revealed by chemogenetic manipulation of the central amygdala, a stress-sensitive nucleus that forms a major input to the DR. Activation of amygdalar corticotropin releasing hormone (CRH)+ neurons abolished the increase in DRv TPH2+ neurons and ameliorated stress-induced anhedonia in susceptible rats. These findings show that activation of amygdalar CRH+ neurons induces resilience, and suppresses the gain of serotonergic phenotype in the DR that is characteristic of susceptible rats. This molecular signature of vulnerability to stress-induced anhedonia and the active nature of resilience could be targeted to develop new treatments for stress-related disorders like depression.
SIGNIFICANCE STATEMENT
Depression and other mental disorders can be induced by chronic or traumatic stressors. However, some individuals are resilient and do not develop depression in response to chronic stress. A complete picture of the molecular differences between susceptible and resilient individuals is necessary to understand how plasticity of limbic circuits is associated with the pathophysiology of stress-related disorders. Using a rodent model, our study identifies a novel molecular marker of susceptibility to stress-induced anhedonia, a core symptom of depression, and a means to modulate it. These findings will guide further investigation into cellular and circuit mechanisms of resilience, and the development of new treatments for depression.







