Summary: For over two decades, the quest to answer “why we sleep” has shifted from psychology to the deep molecular mechanics of our cells. New research reveals that sleep is essentially a metabolic rescue mission for our neurons. During the day, the brain’s “powerhouses” (mitochondria) produce energy but also generate toxic byproducts called reactive oxygen species.
Without sleep, this oxidative damage builds up, threatening the very structures that keep us thinking. Scientists have now discovered that sleep facilitates a “hand-off” where damaged lipids are moved from neurons to supporting glia cells, which then pass them into the blood for final disposal. This process keeps our internal energy sources clean and functional.
Key Facts
- The Energy Cost: Wakefulness causes a buildup of metabolic waste; sleep is the only time the brain can effectively “clean house” by clearing oxidized lipids.
- Mitochondrial Protection: Sleep is vital for maintaining the integrity of mitochondria, the structures that provide the energy for neuronal firing.
- Glia as Janitors: Damaged lipids are transferred from neurons to glial cells during sleep. The glia either burn these lipids for energy or export them into the bloodstream.
- Autophagy Link: Slumber regulates autophagy—the cellular recycling program that turns over old or damaged organelles to keep cells healthy.
- Alzheimer’s Connection: The study found that this “waste removal” uses lipid carriers similar to APOE. In humans, certain versions of the APOE gene (linked to high Alzheimer’s risk) are less effective at this transfer, suggesting sleep deprivation directly accelerates neurodegeneration.
Source: HHMI
When HHMI Investigator Amita Sehgal started studying sleep 25 years ago, the topic elicited a yawn from most biologists.
“In the year 2000, if I had suggested to my department that we hire people working on sleep, they would have laughed at me,” says Sehgal, a molecular biologist and neuroscientist at the University of Pennsylvania.
“The thinking was that sleep is not something that neuroscientists do; psychologists study sleep and dreams.”

Now, more than two decades later, sleep science has finally woken up.
Biologists around the world are now studying sleep in everything from fruit flies to jellyfish to understand the fundamental molecular and cellular mechanisms that drive slumber and answer the age-old question of why we sleep.
“Sleep is widely conserved across the animal kingdom and so it must have some basic function that is the same across species, and so what is that?” Sehgal says. “We’re finally getting to a point where we are recognizing a few basic principles about sleep.”
Sleep Keeps the Brain’s Powerhouses Healthy
Sehgal and her team were among the first to use fruit flies to study the cellular and molecular processes driving the need to sleep.
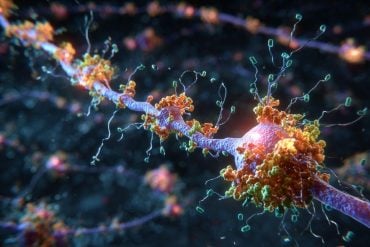
The team’s recent research suggests that the drivers of sleep are metabolic and that sleep plays a key role in protecting the integrity of mitochondria — the structures that power brain cells.
When we are awake, our neurons are constantly firing, powered by the energy produced by mitochondria. A byproduct of this energy production is reactive oxygen species, which can cause damage to the mitochondria and the cells that house them.
Sehgal and her team found that sleep helps neurons stay healthy by facilitating the movement of this oxidative damage to glia cells — a type of supporting cell in the brain — in the form of oxidized lipids. The glia break down some of these lipids to generate energy. They also pass along some of the lipids to blood cells, which have specific receptors to receive them.
“You need those neurons to be functional, and for them to functional, they need a reliable internal source of clean energy,” Sehgal says. “One of the ways that sleep is helping the neurons stay healthy is by moving these lipids along to remove some of the oxidative damage.”
Sleep is a Cellular Housekeeper
In addition to these findings, other recent research by Sehgal and her team shows:
- Sleep regulates autophagy, a process that turns over cellular organelles, including mitochondria, that helps cells stay healthy.
- Sleep promotes the movement of molecules from the brain to the blood through the blood brain barrier.
- Neuromodulators — molecules that activate or silence neurons — are affected by changes in sleep, but they don’t necessarily drive the need to sleep.
- Whether an animal has eaten determines the type of memory it uses — sleep-dependent or sleep-independent.
These findings all support the team’s hypothesis that sleep is driven by metabolic needs. When we don’t sleep, metabolic waste builds up in the brain, meaning neurons — and the energy-generating neuronal mitochondria — can’t function properly.
“We are super excited about our research right now,” Sehgal says. “We feel like we’re sort of really starting to crack the whole sleep thing.”
A Link to Neurodegeneration
The team’s findings on sleep regulation could help researchers better understand neurodegenerative diseases like Alzheimer’s, which are commonly associated with disordered sleep.
Two processes that Sehgal’s lab has shown are regulated by sleep — lipid metabolism and autophagy — are also known to contribute to neurodegeneration when they go awry, and both are disrupted in patients with Alzheimer’s disease.
In flies, the team found that damage is transferred from neurons to glial cells via lipid carriers similar to apolipoprotein E (APOE). In humans, a form of APOE that increases Alzheimer’s risk is less effective at transferring lipids from neurons to glia, suggesting a possible link.
Understanding how sleep influences these cellular processes could help shed light on how their disruption also contributes to Alzheimer’s disease.
“In our very basic work on sleep, we’re finding processes that are regulated by sleep, and that are relevant to and disrupted in Alzheimer’s,” Sehgal says. “The sleep disruption in Alzheimer’s could account for disruption of these two processes.”
Key Questions Answered:
A: According to this research, yes. When you stay awake, your mitochondria continue to produce toxic waste. Sleep is the biological window where those “trash bags” (oxidized lipids) are handed off to janitor cells for disposal. Without that window, the toxins accumulate inside your neurons.
A: While it’s not a cure, the study shows that the processes used to clean the brain during sleep are the same ones that fail in Alzheimer’s patients. Maintaining healthy sleep hygiene helps ensure your brain’s waste-clearance system (the glymphatic and lipid transfer systems) is working at full capacity.
A: Sleep is ancient and conserved across almost the entire animal kingdom. By studying fruit flies, scientists can isolate the basic genetic “switches” that control metabolism and cell repair, which work remarkably similarly in the human brain.
Editorial Notes:
- This article was edited by a Neuroscience News editor.
- Journal paper reviewed in full.
- Additional context added by our staff.
About this sleep and neuroscience research news
Author: Nanci Bompey
Source: HHMI
Contact: Nanci Bompey – HHMI
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Sleep-dependent clearance of brain lipids by peripheral blood cells” by Bumsik Cho, Diane E. Youngstrom, Samantha Killiany, Camilo Guevara, Caitlin E. Randolph, Connor H. Beveridge, Pooja Saklani, Gaurav Chopra & Amita Sehgal. Nature
DOI:10.1038/s41586-025-10050-w
Abstract
Sleep-dependent clearance of brain lipids by peripheral blood cells
Sleep is viewed typically through a brain-centric lens, with little known about the role of the periphery.
Here we identify a sleep function for peripheral macrophage-like cells (haemocytes) in the Drosophila circulation, showing that haemocytes track to the brain during sleep and take up lipids accumulated in cortex glia due to wake-associated oxidative damage.
Through a screen of phagocytic receptors expressed in haemocytes, we discovered that knockdown of eater—a member of the Nimrod receptor family—reduces sleep. Loss of eater also disrupts haemocyte localization to the brain and lipid uptake, which results in increased brain levels of acetyl-CoA and acetylated proteins, including mitochondrial proteins PGC1α and DRP1.
Dysregulation of mitochondria, reflected in high oxidation and reduced NAD+, is accompanied by impaired memory and lifespan.
Thus, peripheral blood cells, which we suggest are precursors of mammalian microglia, perform a daily function of sleep to maintain brain function and fitness.