Summary: Habitual short sleepers might be more efficient sleepers, but also more tired than they realize, a new study reports.
Source: University of Utah.
Most people could benefit from a few extra hours of sleep every night. But some people habitually sleep much less than the recommended amount, yet report feeling no ill effects. A new University of Utah study, published Sept. 15 in Brain and Behavior, finds that patterns of neural connections in the brains of so-called “habitual short sleepers” suggest that some of these people may be efficient sleepers, but may also be more tired than they realize.
“This is tantalizing evidence for why some people feel like they don’t need to sleep as much,” says study co-author and radiologist Jeff Anderson. “Maybe some brains are able to do what sleep does in little tiny epochs during the day.”
Why we sleep
The reasons for sleep are still a mystery. “It’s one of the most interesting questions in all science: Why do we sleep in the first place?” Anderson says. “It’s incredibly disadvantageous to spend a third of our life asleep. There must be an important reason to do it, but why is still an active field of research.”
Some of the leading hypotheses hold that sleep clears the brain of compounds accumulated throughout the day, and allows memories to move from short-term to long-term memory storage.
For most people, getting less than the recommended seven to nine hours of sleep a night results in fatigue, irritability and some impairment in judgment and reasoning. Long-term short sleep duration has been linked to a host of mental and physical health consequences, including diminished cognitive performance, mood disturbance, obesity, coronary disease and all-cause mortality risk.
But some people who get less than six hours of sleep a night report feeling no ill effects. In 2009, University of Utah neurologist Christopher Jones and colleagues found a rare genetic mutation that was associated with short-duration, efficient sleep. Many genetic factors are involved in sleep, and a combination of such factors may lead some people to feel that they need less sleep than others.
“Most people feel terrible when they get less than six hours of sleep,” says study co-author and psychology professor Paula Williams. “What’s different about these short sleepers who feel fine? Is there something different going on in terms of brain function? Although they report no daytime dysfunction from short sleep, what if their perceptions are inaccurate?”
The brain’s wiring diagram
To begin answering those questions, Williams, Anderson, Jones and psychology graduate student Brian Curtis, who is first author on the new study, looked into how people’s brains are wired together. “Most of the cells in the brain are just a little thin layer of gray matter cells along the surface,” Anderson says. “Everything else in the middle are connections between those points on the surface and a few way stations in between. So figuring out where those connections go, which points are connected and which points aren’t in the gray matter is really everything about how the brain works.”
The set of brain connections, also called the “connectome” is currently being explored with the Human Connectome Project, a multiuniversity consortium analyzing the network of connections in 1,200 people through MRI scans. So far, data from about 900 people have been released, allowing researchers like those at the University of Utah access to a large dataset of brain connectivity.
Cat-napping?
The team compared data from people who reported a normal amount of sleep in the past month with those who reported sleeping six hours or less a night. They further divided the short sleepers into two groups: Those who reported daytime dysfunction, such as feeling too drowsy to perform common tasks or keeping up enthusiasm, and those who reported feeling fine.
Both groups of short sleepers exhibited connectivity patterns more typical of sleep than wakefulness while in the MRI scanner. Anderson says that although people are instructed to stay awake while in the scanner, some short sleepers may have briefly drifted off, even those who denied dysfunction. “People are notoriously poor at knowing whether they’ve fallen asleep for a minute or two,” he says. For the short sleepers who deny dysfunction, one hypothesis is that their wake-up brain systems are perpetually in over-drive. “This leaves open the possibility that, in a boring fMRI scanner they have nothing to do to keep them awake and thus fall asleep,” says Jones. This hypothesis has public safety implications, according to Curtis. “Other boring situations, like driving an automobile at night without adequate visual or auditory stimulation, may also put short sleepers at risk of drowsiness or even falling asleep behind the wheel,” he says.
Looking specifically at differences in connectivity between brain regions, the researchers found that short sleepers who denied dysfunction showed enhanced connectivity between sensory cortices, which process external sensory information, and the hippocampus, a region associated with memory. “That’s tantalizing because it suggests that maybe one of the things the short sleepers are doing in the scanner is performing memory consolidation more efficiently than non-short sleepers,” Anderson says. In other words, some short sleepers may be able to perform sleep-like memory consolidation and brain tasks throughout the day, reducing their need for sleep at night. Or they may be falling asleep during the day under low-stimulation conditions, often without realizing it.
Testing perceptions of dysfunction
The next phase of the team’s research, to be conducted at the University of Utah, will directly test whether short sleepers who deny dysfunction are actually doing fine. “Most people who are deprived of sleep show cognitive impairment similar to being intoxicated,” Williams says. However, prior research has largely involved experimental sleep restriction of normal sleepers. The researchers plan to recruit individuals who naturally sleep less than six hours a night, regardless of whether it is the weekend, workday or vacation. In addition to brain imaging, they will examine cognitive performance, including driving simulator testing, to get objective information about functioning. Getting insufficient sleep may affect people’s perception of their own dysfunction, Williams says. “We are particularly interested in understanding the discrepancy between people’s perception of their functioning and how they’re actually functioning. Not everyone is equally accurate.” The team’s future work will also incorporate reports by the study subjects’ family members or partners, to provide an additional evaluation of daytime function.
What it means
In analyzing connectome data, the team found that self-reported average sleep duration over the prior month was the factor that best accounted for the variation between people’s resting connectivity profiles. Anderson says this result suggests future fMRI studies should take sleep into account when interpreting results. “Sleep is central to everything we do,” he says. “All psychiatric disorders are impacted by sleep.”
Williams hopes that this ongoing research program will answer key questions about individual differences in need for sleep. “Two people can sleep the same amount and one person feels refreshed and one does not,” she says. “What’s the difference? Are there some people who can get away with less sleep? We don’t know. Amazingly, we still don’t know.”
Source: Paula Williams – University of Utah
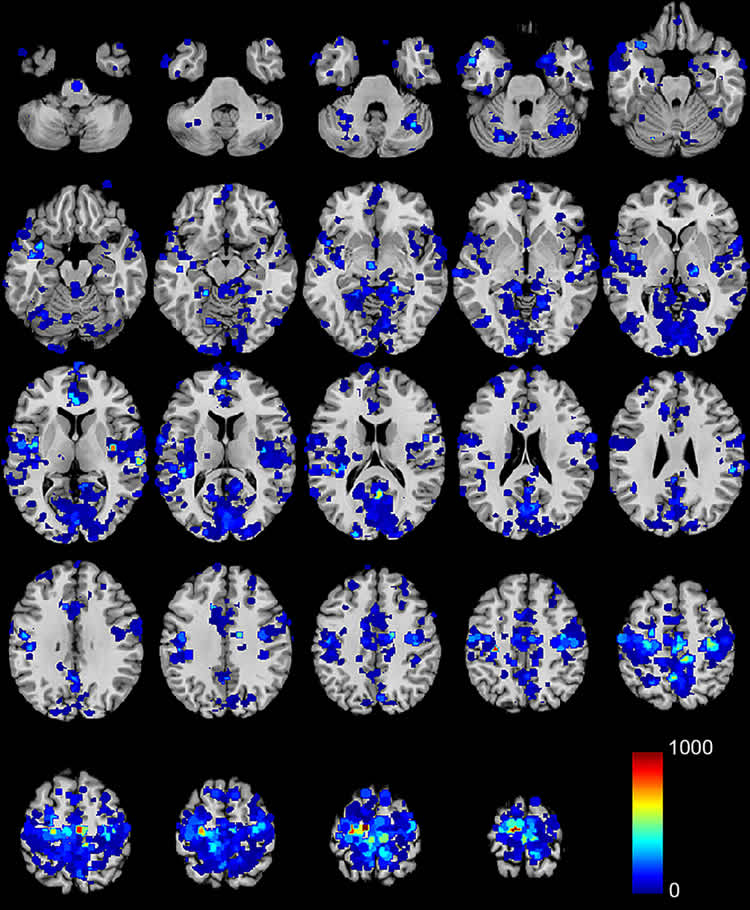
Image Source: NeuroscienceNews.com image is credited to Williams et al./Brain and Behavior.
Original Research: Full open access research for “Sleep duration and resting fMRI functional connectivity: examination of short sleepers with and without perceived daytime dysfunction” by Brian J. Curtis, Paula G. Williams, Christopher R. Jones, and Jeffrey S. Anderson in Brain and Behavior. Published online September 15 2016 doi:10.1002/brb3.576
[cbtabs][cbtab title=”MLA”]University of Utah. “Looking Into the Brains of Habitual Short Sleepers.” NeuroscienceNews. NeuroscienceNews, 16 September 2016.
<https://neurosciencenews.com/short-sleepers-neuroscience-5062/>.[/cbtab][cbtab title=”APA”]University of Utah. (2016, September 16). Looking Into the Brains of Habitual Short Sleepers. NeuroscienceNews. Retrieved September 16, 2016 from https://neurosciencenews.com/short-sleepers-neuroscience-5062/[/cbtab][cbtab title=”Chicago”]University of Utah. “Looking Into the Brains of Habitual Short Sleepers.” https://neurosciencenews.com/short-sleepers-neuroscience-5062/ (accessed September 16, 2016).[/cbtab][/cbtabs]
Abstract
Sleep duration and resting fMRI functional connectivity: examination of short sleepers with and without perceived daytime dysfunction
Background
Approximately 30% of the U.S. population reports recurrent short sleep; however, perceived sleep need varies widely among individuals. Some “habitual short sleepers” routinely sleep 4–6 hr/night without self-reported adverse consequences. Identifying neural mechanisms underlying individual differences in perceived sleep-related dysfunction has important implications for understanding associations between sleep duration and health.
Method
This study utilized data from 839 subjects of the Human Connectome Project to examine resting functional connectivity associations with self-reported short sleep duration, as well as differences between short sleepers with versus without reported dysfunction. Functional connectivity was analyzed using a parcellation covering the cortical, subcortical, and cerebellar gray matter at 5 mm resolution.
Results
Self-reported sleep duration predicts one of the primary patterns of intersubject variance in resting functional connectivity. Compared to conventional sleepers, both short sleeper subtypes exhibited resting fMRI (R-fMRI) signatures consistent with diminished wakefulness, potentially indicating inaccurate perception of functionality among those denying dysfunction. Short sleepers denying dysfunction exhibited increased connectivity between sensory cortices and bilateral amygdala and hippocampus, suggesting that efficient sleep-related memory consolidation may partly explain individual differences in perceived daytime dysfunction.
Conclusions
Overall, current findings indicate that R-fMRI investigations should include assessment of average sleep duration during the prior month. Furthermore, short sleeper subtype findings provide a candidate neural mechanism underlying differences in perceived daytime impairment associated with short sleep duration.
“Sleep duration and resting fMRI functional connectivity: examination of short sleepers with and without perceived daytime dysfunction” by Brian J. Curtis, Paula G. Williams, Christopher R. Jones, and Jeffrey S. Anderson in Brain and Behavior. Published online September 15 2016 doi:10.1002/brb3.576






