Summary: A new study reveals probiotic use can result in a significant accumulation of bacteria in the small intestine. Researchers say the bacterial accumulation can result in brain fogginess and significant belly bloating.
Source: Medical College of Georgia at Augusta University.
Probiotic use can result in a significant accumulation of bacteria in the small intestine that can result in disorienting brain fogginess as well as rapid, significant belly bloating, investigators report.
In a published study of 30 patients, the 22 who reported problems like confusion and difficulty concentrating, in addition to their gas and bloating, were all taking probiotics, some several varieties.
When investigators looked further, they found large colonies of bacteria breeding in the patients’ small intestines, and high levels of D-lactic acid being produced by the bacteria lactobacillus’ fermentation of sugars in their food, says Dr. Satish S.C. Rao, director of neurogastroenterology/motility and the Digestive Health Clinical Research Center at the Medical College of Georgia at Augusta University.
D-lactic acid is known to be temporarily toxic to brain cells, interfering with cognition, thinking and sense of time. They found some patients had two to three times the normal amount of D-lactic acid in their blood. Some said their brain fogginess – which lasted from a half hour to many hours after eating – was so severe that they had to quit their jobs.
The report in the journal Clinical and Translational Gastroenterology appears to be the first time the connection has been made between brain fogginess, bacterial overgrowth in the small intestine, high levels of D-lactic acid in the gut and probiotic use, Rao says.
“What we now know is that probiotic bacteria have the unique capacity to break down sugar and produce D-lactic acid. So if you inadvertently colonize your small bowel with probiotic bacteria, then you have set the stage for potentially developing lactic acidosis and brain fogginess,” Rao says.
While probiotics can be beneficial in some scenarios, like helping a patient restore his gut bacteria after taking antibiotics, the investigators advised caution against its excessive and indiscriminate use.
“Probiotics should be treated as a drug, not as a food supplement,” Rao says, noting that many individuals self-prescribe the live bacteria, which are considered good for digestion and overall health.
Others have implicated probiotics in the production of D-lactic acid – and brain fogginess – in patients with a short bowel so their small intestine does not function properly, and in newborns fed formula containing the popular product. Short bowel syndrome results in a lot of undigested carbohydrates that are known to cause small intestinal bacterial overgrowth, or SIBO, and the high levels of D-lactic acid. Severe liver and kidney problems can produce similar problems.
Whether there was also a connection when the gut is intact was an unknown. “This is the first inroad,” says Rao.
All patients experiencing brain fogginess took probiotics and SIBO was more common in the brain fogginess group as well, 68 percent compared to 28 percent, respectively. Patients with brain fogginess also had a higher prevalence of D-lactic acidosis, 77 versus 25 percent, respectively.
When brain-foggy patients stopped taking probiotics and took a course of antibiotics, their brain fogginess resolved.
Movement of food through the gastrointestinal tract was slow in one third of the brain foggy patients and one fourth of the other group. Slower passage, as well as things like obesity surgery, can increase the chance of bacterial buildup, or SIBO.
“Now that we can identify the problem, we can treat it,” Rao says. Diagnosis includes breath, urine and blood tests to detect lactic acid, and an endoscopy that enables examination of fluid from the small intestines so the specific bacteria can be determined and the best antibiotics selected for treatment.
Normally there is not much D-lactic acid made in the small intestines, but probiotic use appears to change that. SIBO, which was present in most with brain fogginess, can cause bacteria to go into a feeding frenzy that ferments sugars resulting in production of uncomfortable things like hydrogen gas and methane that explain the bloating.
Probiotics added to that feeding frenzy the bacterium lactobacillus, which produces D-lactic acid as it breaks down sugars, The acid get absorbed in the blood and can reach the brain.
All those with brain fogginess, SIBO and/or D-lactic acidosis, were given antibiotics that targeted their bacterial population and asked to discontinue probiotics. Those without SIBO were asked to halt probiotics and stop eating yogurt, which is considered one of the best sources of probiotics. Those with SIBO and D-lactic acidosis but no brain fogginess also took antibiotics.
Following treatment, 70 percent of patients reported significant improvement in their symptoms and 85 percent said their brain fogginess was gone. Those without brain fogginess but with SIBO and high levels of D-lactic acid reported significant improvement in symptoms like bloating and cramping within three months.
Abdominal pain was the most common symptom in both groups and before treatment, six of those with brain fogginess reported a tremendous increase in their abdominal size within just a few minutes of eating.
All patients received extensive examination of their gastrointestinal tract, including a motility test, to rule out other potential causes of their symptoms. They filled out questionnaires about symptoms like abdominal pain, belching and gas and answered questions about related issues like antibiotic and probiotic use as well as food fads and yogurt consumption.
They were given carbohydrates followed by extensive metabolic testing looking at the impact on things like blood glucose and insulin levels. Levels of D-lactic acid and L-lactate acid, which results from our muscles’ use of glucose as energy and can cause muscle cramps, also were measured.
Probiotic use may be particularly problematic for patients who have known problems with motility, as well as those taking opioids and proton pump inhibitors, which reduce stomach acid secretion and so the natural destruction of excessive bacteria.
Probiotics are supposed to work in the colon and not the small intestines or stomach, Rao says, so motility issues can result in problems with probiotic bacteria reaching the proper place. A wide variety of problems, from conditions like diabetes to drugs like antidepressants and minerals like iron, can slow movement and increase the possibility that probiotics will remain too long in the upper gut where they can cause harm, he says.
Probiotics definitely can help, for example, people who have gastroenteritis, or stomach flu, or are left with diarrhea and other problems after antibiotics wipe out their natural gut bacteria, Rao says.
“In those situations, we want to build up their bacterial flora so probiotics are ideal,” he says.
Rao’s pursuit of a possible connection between probiotics, brain fogginess and bloating started with a memorable patient who developed significant amounts of both problems within a minute of eating.
“It happened right in front of our eyes,” Rao says of the dramatic abdominal distention. They knew the woman had diabetes, which can slow motility. When they looked in the blood and urine at a variety of metabolic compounds, they found the high levels of D-lactic acid and soon learned the patient used probiotics and regularly ate yogurt.
Next steps include additional studies in which the investigators better quantify and characterize the brain fogginess reported by patients and following patients for longer periods to ensure their problems remain resolved. Some patients in the current study required a couple of rounds of antibiotics, Rao notes.
Good food sources of probiotics include yogurt, sauerkraut, kimchi, kefir and dark chocolate, which are generally safe because of the small amounts of bacteria present, Rao says.
The 19-foot long small intestine has been a bit of an understudied organ, likely in part because it’s hard to visualize via the mouth or anus, Rao says. “I think the small bowel can be a source of huge mystery,” Rao says.
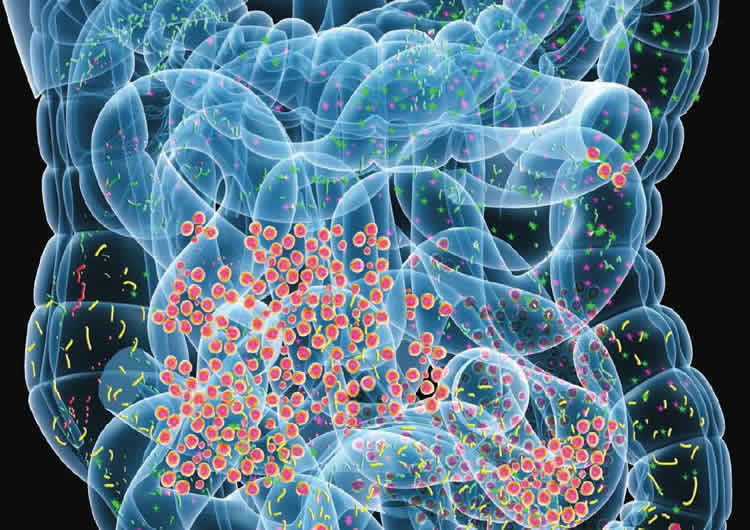
Your helpful gut bacteria, or microbiome, which are essential to things like a well-functioning immune system and general health, are largely in the large intestine and colon.
Source: Toni Baker – Medical College of Georgia at Augusta University
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Open access research for “Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis” by Satish S. C. Rao, Abdul Rehman, Siegfried Yu & Nicole Martinez de Andino in Clinical and Translational Gastroenterology. Published June 19 2018.
doi:10.1038/s41424-018-0030-7
[cbtabs][cbtab title=”MLA”]Medical College of Georgia at Augusta University”Probiotic Use is a Link Between Brain Fogginess and Severe Bloating.” NeuroscienceNews. NeuroscienceNews, 6 August 2018.
<https://neurosciencenews.com/probiotics-brain-fog-bloating-9659/>.[/cbtab][cbtab title=”APA”]Medical College of Georgia at Augusta University(2018, August 6). Probiotic Use is a Link Between Brain Fogginess and Severe Bloating. NeuroscienceNews. Retrieved August 6, 2018 from https://neurosciencenews.com/probiotics-brain-fog-bloating-9659/[/cbtab][cbtab title=”Chicago”]Medical College of Georgia at Augusta University”Probiotic Use is a Link Between Brain Fogginess and Severe Bloating.” https://neurosciencenews.com/probiotics-brain-fog-bloating-9659/ (accessed August 6, 2018).[/cbtab][/cbtabs]
Abstract
Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis
Background
D-lactic acidosis is characterized by brain fogginess (BF) and elevated D-lactate and occurs in short bowel syndrome. Whether it occurs in patients with an intact gut and unexplained gas and bloating is unknown. We aimed to determine if BF, gas and bloating is associated with D-lactic acidosis and small intestinal bacterial overgrowth (SIBO).
Methods
Patients with gas, bloating, BF, intact gut, and negative endoscopic and radiological tests, and those without BF were evaluated. SIBO was assessed with glucose breath test (GBT) and duodenal aspiration/culture. Metabolic assessments included urinary D-lactic acid and blood L-lactic acid, and ammonia levels. Bowel symptoms, and gastrointestinal transit were assessed.
Results
Thirty patients with BF and 8 without BF were evaluated. Abdominal bloating, pain, distension and gas were the most severe symptoms and their prevalence was similar between groups. In BF group, all consumed probiotics. SIBO was more prevalent in BF than non-BF group (68 vs. 28%, p = 0.05). D-lactic acidosis was more prevalent in BF compared to non-BF group (77 vs. 25%, p = 0.006). BF was reproduced in 20/30 (66%) patients. Gastrointestinal transit was slow in 10/30 (33%) patients with BF and 2/8 (25%) without. Other metabolic tests were unremarkable. After discontinuation of probiotics and a course of antibiotics, BF resolved and gastrointestinal symptoms improved significantly (p = 0.005) in 23/30 (77%).
Conclusions
We describe a syndrome of BF, gas and bloating, possibly related to probiotic use, SIBO, and D-lactic acidosis in a cohort without short bowel. Patients with BF exhibited higher prevalence of SIBO and D-lactic acidosis. Symptoms improved with antibiotics and stopping probiotics. Clinicians should recognize and treat this condition.







