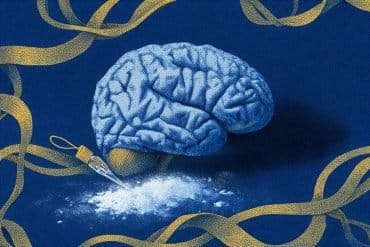
Summary: The microbial ecosystems in our mouths may impact cognitive function as we age, with pathogenic bacteria linked to cognitive decline. Researchers found that beneficial bacteria, such as Neisseria, are associated with improved memory and attention, while harmful bacteria like Porphyromonas correlate with mild cognitive impairment.
These findings suggest that diet, particularly nitrate-rich foods, could promote beneficial bacteria and support brain health. Further research may reveal how oral health interventions could help delay cognitive decline and reduce the risk of dementia or Alzheimer’s disease.
Key Facts:
- Microbial Connection: Beneficial oral bacteria, like Neisseria, support cognitive functions, while harmful bacteria, such as Porphyromonas, predict cognitive decline.
- Dietary Influence: A nitrate-rich diet fosters beneficial oral bacteria linked to better cognitive outcomes.
- APOE4 Link: Specific harmful bacteria (Prevotella intermedia) are associated with the APOE4 allele, a known risk factor for Alzheimer’s.
Source: PNAS Nexus
The microbial ecosystems within our mouths may affect our cognitive function as we age, according to a study. Interventions such as prebiotics, including dietary nitrate, have potential for delaying cognitive decline.
About 15% of older adults have mild cognitive impairment, which is the largest risk factor for the development of dementia or Alzheimer’s disease. There is a known association between periodontitis—gum disease—and worsened cognitive function.

Researchers have identified two possible links between the mouth and the mind: pathogenic oral bacteria could enter the bloodstream and move to the brain, or pathogenic oral bacteria could displace nitrate-reducing bacteria, which help create nitric oxide the brain needs for synaptic plasticity and long-term potentiation.
Anni Vanhatalo and colleagues characterized the oral microbiome of 115 participants, 55 of whom had mild cognitive impairment.
Some participants had the apolipoprotein E4 (APOE4) allele, which increases risk for cognitive decline and Alzheimer’s disease.
A high relative abundance of bacteria in the genus Neisseria was associated with better executive function and visual attention within the mild cognitive impairment group.
Among healthy participants, Neisseria correlated with working memory.
High prevalence of bacteria in the genus Porphyromonas predicted mild cognitive impairment status, while Prevotella intermedia predicted APOE4-carrier status.
According to the authors, diet can affect the oral microbiome, and a nitrate-rich diet (such as the Mediterranean and ‘Dietary Approaches to Stop Hypertension’ diets), favors bacteria associated with good cognitive outcomes.
About this cognition and neuroscience research news
Author: Anni Vanhatalo
Source: PNAS Nexus
Contact: Anni Vanhatalo – PNAS Nexus
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Oral microbiome and nitric oxide biomarkers in older people with mild cognitive impairment and APOE4 genotype” by Anni Vanhatalo et al. PNAS Nexus
Abstract
Oral microbiome and nitric oxide biomarkers in older people with mild cognitive impairment and APOE4 genotype
Apolipoprotein E4 (APOE4) genotype and nitric oxide (NO) deficiency are risk factors for age-associated cognitive decline. The oral microbiome plays a critical role in maintaining NO bioavailability during aging.
The aim of this study was to assess interactions between the oral microbiome, NO biomarkers, and cognitive function in 60 participants with mild cognitive impairment (MCI) and 60 healthy controls using weighted gene co-occurrence network analysis and to compare the oral microbiomes between APOE4 carriers and noncarriers in a subgroup of 35 MCI participants.
Within the MCI group, a high relative abundance of Neisseria was associated with better indices of cognition relating to executive function (Switching Stroop, rs = 0.33, P = 0.03) and visual attention (Trail Making, rs = −0.30, P = 0.05), and in the healthy group, Neisseria correlated with working memory (Digit Span, rs = 0.26, P = 0.04). High abundances of Haemophilus (rs = 0.38, P = 0.01) and Haemophilus parainfluenzae (rs = 0.32, P = 0.03), that co-occurred with Neisseria correlated with better scores on executive function (Switching Stroop) in the MCI group.
There were no differences in oral nitrate (P = 0.48) or nitrite concentrations (P = 0.84) between the MCI and healthy groups. Linear discriminant analysis Effect Size identified Porphyromonas as a predictor for MCI and Prevotella intermedia as a predictor of APOE4-carrier status.
The principal findings of this study were that a greater prevalence of oral P. intermedia is linked to elevated genetic risk for dementia (APOE4 genotype) in individuals with MCI prior to dementia diagnosis and that interventions that promote the oral Neisseria–Haemophilus and suppress Prevotella-dominated modules have potential for delaying cognitive decline.