Summary: A new study has revealed that newborn babies and Alzheimer’s patients both have elevated levels of the same protein, p-tau217, in their blood. While this protein is a key marker of brain degeneration in Alzheimer’s, in newborns it appears to support healthy brain growth and development.
The highest levels were seen in premature infants and dropped steadily after birth, suggesting a role in early brain wiring. Understanding how infants manage these high tau levels without harm could help unlock new strategies to prevent or treat Alzheimer’s.
Key Facts:
- Shared Biomarker: Newborns and Alzheimer’s patients both show high levels of p-tau217 in their blood.
- Different Mechanisms: In babies, elevated p-tau217 supports brain development—unlike in Alzheimer’s, where it signals pathology.
- Therapeutic Clues: Studying newborn resilience to tau may offer insights for future Alzheimer’s therapies.
Source: University of Gothenburg
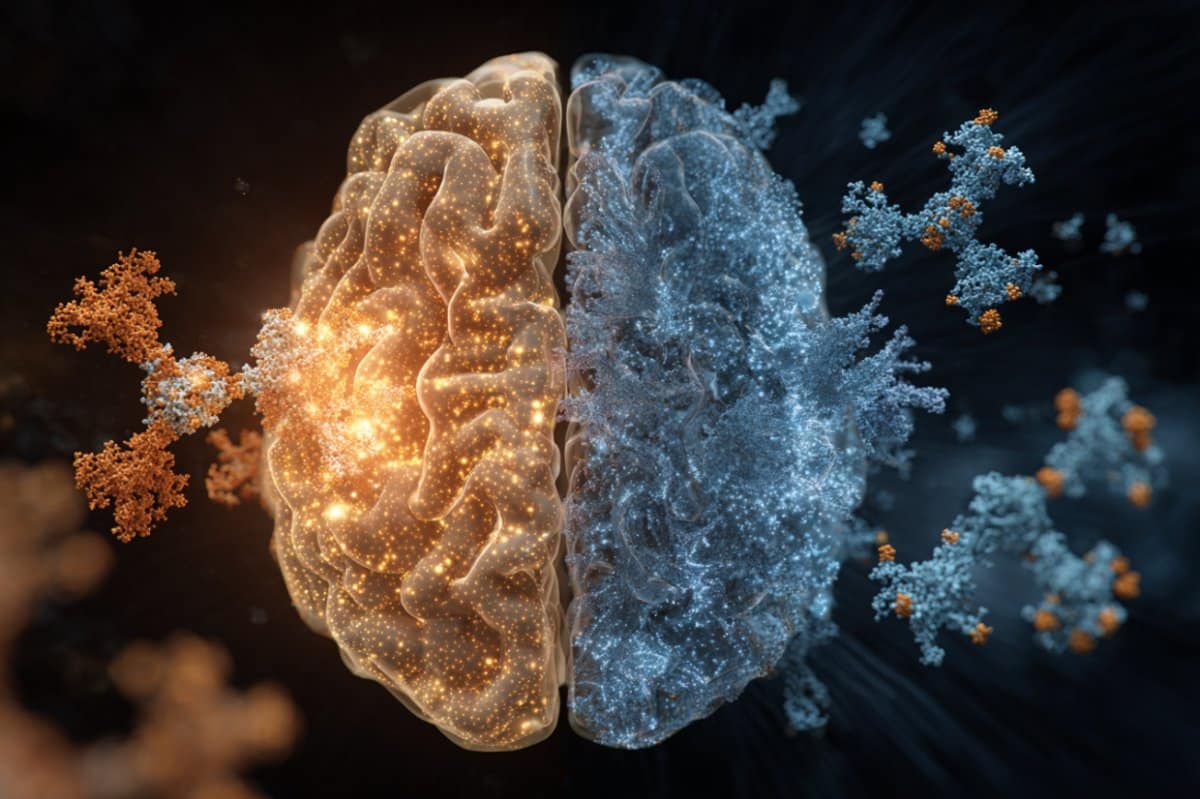
What do the brains of newborns and patients with Alzheimer’s disease have in common?
Researchers from the University of Gothenburg, led by first author Fernando Gonzalez-Ortiz and senior author Professor Kaj Blennow, recently reported that both newborns and Alzheimer’s patients have elevated blood levels of a protein called phosphorylated tau, specifically a form called p-tau217.
While this protein has been largely used as a diagnostic test for Alzheimer’s disease, with an increase in p-tau217 blood levels proposed to be driven by another process, namely aggregation of b-amyloid protein into amyloid plaques.
Newborns (for natural reasons) do not have this type of pathological change, so interestingly, in newborns increased plasma p-tau217 seems to reflect a completely different – and entirely healthy – mechanism.
In a large international study that involved Sweden, Spain and Australia, researchers analyzed blood samples from over 400 individuals, including healthy newborns, premature infants, young adults, elderly adults, and people diagnosed with Alzheimer’s disease.
They found that newborn babies had the highest levels of p-tau217 – even higher than those found in people with Alzheimer’s. These levels were particularly elevated in premature babies and started to decrease over the first few months of life, eventually settling to adult levels.
First time in the blood of newborns
Previous research, largely based on animal models, had hinted at the role of phosphorylated tau in early brain development. This is the first time scientists have directly measured p-tau217 concentrations in the blood of human newborns, opening the door to a much clearer understanding of its developmental role.
But here’s where it gets fascinating, while in Alzheimer’s disease p-tau217 is associated with tau aggregation into harmful clumps called tangles, believed to cause the breakdown of brain cells and subsequent cognitive decline.
In contrast, in newborns this surge in tau appears to support healthy brain development, helping neurons grow and to form new connections with other neurons, thereby shaping the structure of the young brain.
The study also revealed that in both healthy and premature babies, p-tau217 levels were closely linked to how early they were born. The earlier the birth, the higher the levels of this protein, suggesting a role in supporting rapid brain growth under challenging developmental conditions.
Potential roadmap for new treatments
What’s perhaps most compelling about these findings, published in the journal Brain Communications, is the hint that our brains may once have had built-in protection against the damaging effects of tau, so that newborns can tolerate, and even benefit from, high levels of phosphorylated tau without triggering the kinds of damage seen in Alzheimer’s.
“We believe that understanding how this natural protection works – and why we lose it as we age – could offer a roadmap for new treatments. If we can learn how the newborn brain keeps tau in check, we might one day mimic those processes to slow or stop Alzheimer’s in its tracks”, says Fernando Gonzalez-Ortiz.
So while an increase of p-tau217 is a danger signal in older brains, in newborns it might be a vital part of building one. The same molecule, two dramatically different roles – one building the brain, the other marking its decline.
Plasma p-tau217 has recently received FDA approval for use in diagnosing Alzheimer’s disease, making it an increasingly important tool in clinical settings.
The authors emphasize the need to also understand the mechanism for the increase in p-tau217, especially for interpreting it as an outcome in clinical and epidemiological research and in drug development.
This study indicate that amyloid plaques may not be the main driver of increases in p-tau217.
About this genetics, Alzheimer’s disease, and neurodevelopment research news
Author: Margareta G. Kubista
Source: University of Gothenburg
Contact: Margareta G. Kubista – University of Gothenburg
Image: The image is credited to Neuroscience News
Original Research: Open access.
“The potential dual role of tau phosphorylation: Plasma p-tau217 in newborns and Alzheimer’s disease” by Fernando Gonzalez-Ortiz et al. Brain Communications
Abstract
The potential dual role of tau phosphorylation: Plasma p-tau217 in newborns and Alzheimer’s disease
Tau phosphorylation plays an important role in brain physiology and pathology.
During foetal development, it supports microtubule dynamics and neuroplasticity, whereas in Alzheimer’s disease (AD), it drives pathological tau aggregation and tangle formation.
In this multicentre study (n = 462), we measured plasma phosphorylated-tau217 in healthy newborns, premature infants, patients with AD and healthy controls across various age groups.
Plasma phosphorylated-tau217 levels were significantly higher in newborns compared to healthy individuals of any age group and even exceeded levels observed in patients with AD. In newborns, plasma phosphorylated-tau217 levels inversely correlated with perinatal factors such as gestational age.
Longitudinal analysis of preterm infants demonstrated a decline in serum phosphorylated-tau217 levels over the first months of life, approaching levels observed in young adults.
In contrast, elevated plasma phosphorylated-tau217 in older individuals was associated with AD pathology.
Our findings corroborate the crucial role of tau phosphorylation in early brain development. However, in AD, tau phosphorylation transitions into a pathological mechanism.
The high levels of blood-based phosphorylated-tau217 observed at birth and subsequent clearance might indicate distinct regulatory mechanisms that prevent tau aggregation in early life.
Further studies are needed to explore the shared mechanisms of tau phosphorylation in newborns and AD.