Summary: An immune protein called CSF1 may contribute to feelings of anxiety as a result of alcohol withdrawal for those with alcohol use disorder.
Source: Scripps Research Institute
The anxiety that occurs during withdrawal from excessive alcohol use, and contributes to relapse, may be driven in part by the release of an immune protein in the brain, according to a new study from scientists at Scripps Research.
The discovery, reported online June 6, 2022, in Molecular Psychiatry, illuminates the molecular details of the brain’s response to alcohol withdrawal, and suggests that the immune protein, colony stimulating factor 1 (CSF1), could be a target of future treatments for alcohol use disorder (AUD).
“Alcohol withdrawal activates the stress system in the brain, which contributes to relapse, and in this study, we linked this stress response to CSF1, a neuroimmune mediator, opening up new opportunities for therapeutic intervention,” says study senior author Marisa Roberto, PhD, professor and Schimmel Family Chair in the Department of Molecular Medicine at Scripps Research.
The study’s first author, who performed many of the experiments, is Reesha R. Patel, PhD, a former postdoctoral researcher in the Roberto lab.
Alcohol is by far the most used and abused recreational drug. According to the 2019 National Survey on Drug Use and Health, nine million men and more than five million women in the United States have an alcohol use disorder (AUD), which is defined as an inability to control alcohol use despite its negative impact on the user’s health, social life and/or employment.
Drug treatments, talk-therapy and support group-based treatments are available, but relapse is common, mainly due to the limited understanding of the brain-circuit dysfunctions underlying AUD.
Scientists know that relapse-promoting alcohol withdrawal symptoms include rising feelings of anxiety, caused at least in part by the release of stress molecules such as corticotropin-releasing factor (CRF) within the brain. CRF stimulates receptors on neurons in the prefrontal cortex, and in the limbic system, a set of more primitive brain structures that process emotions.
If scientists could fully identify and characterize these CRF-sensitive neuronal populations, they could understand better how anxiety occurs during withdrawal and potentially devise effective treatments to block it.
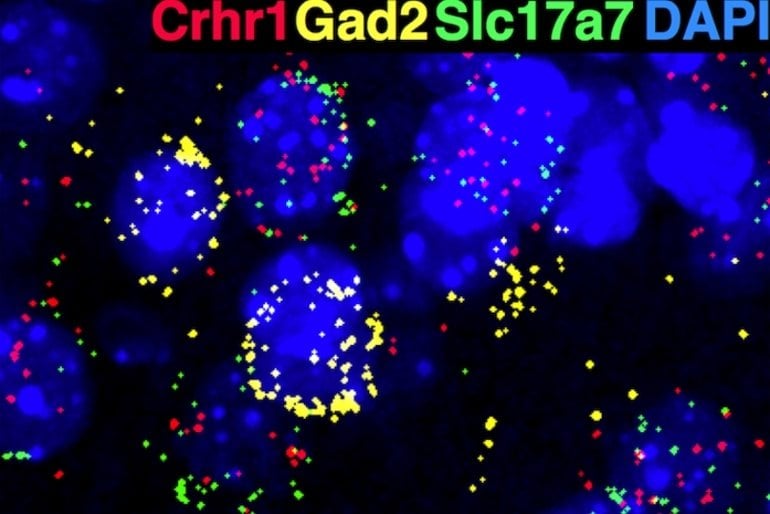
Toward that end, Roberto and her team, in the new study, identified a population of neurons in the medial prefrontal cortex (mPFC) of mice that are sensitive to CRF because they express a CRF receptor called CRF1. The scientists showed that these neurons are involved in altering mood and behavior during alcohol exposure and withdrawal.
The team’s initial experiments revealed that deletion of these CRF-sensitive neurons makes the mice less anxious, suggesting that the neurons normally mediate anxiety-like behaviors.
The researchers subsequently found that these CRF-sensitive mPFC neurons become less excitable—less likely to fire signals to other neurons when stimulated—in alcohol-dependent mice that experience alcohol withdrawal. In contrast, nearby mPFC neurons lacking CRF receptors become more excitable.
“These CRF-sensitive mPFC neurons appear to constitute a unique neuronal population that undergoes profound neuroadaptations with chronic alcohol exposure,” says study co-author Pauravi Gandhi, PhD, a postdoctoral research associate in the Roberto lab.
Intriguingly, the researchers found that alcohol withdrawal, even as it dialed down the excitability of the CRF-sensitive neurons, also induced large increases in CSF1 gene expression within these neurons. CSF1 is an immune protein best known for its role in stimulating stem cells to mature into large white blood cells called macrophages.
In the brain, CSF1 is thought to have a similar role in sustaining brain-resident immune cells called microglia. Moreover, prior research in mice has suggested that under conditions of chronic stress, CSF1 production rises in the mPFC, driving microglia to prune connections between neurons, which in turn causes signs of anxiety and depression.
Looking more closely at CSF1’s role in alcohol withdrawal, Roberto and colleagues artificially increased CSF1 production in CRF-sensitive mPFC neurons in mice, and observed that the animals exhibited many of the same neuronal and behavioral changes seen in alcohol withdrawal—suggesting that elevated CSF1 levels in mPFC may be a key driver of alcohol-withdrawal signs and symptoms.
“Targeting CSF1 therefore may be a good strategy for treating AUD, and we’re now eager to test that in our preclinical models,” Patel says.
“Ethanol withdrawal-induced adaptations in prefrontal corticotropin releasing factor receptor 1-expressing neurons regulate anxiety and conditioned rewarding effects of ethanol” was co-authored by Reesha Patel, Sarah Wolfe, Vittoria Borgonetti, Pauravi Gandhi, Larry Rodriguez, Angela Snyder, Shannon D’Ambrosio, Michal Bajo, Alain Domissy, Steven Head, Candice Contet, R. Dayne Mayfield, Amanda Roberts and Marisa Roberto.
Funding: The research was supported by the National Institutes of Health (AA021491, AA017447, AA015566, AA006420, AA013498, AA026685, AA027700, AA029841, K99 AA029180, F32 AA026765, T32 AA007456) and by the Pearson Center for Alcoholism and Addiction Research.
About this alcohol use disorder research news
Author: Press Office
Source: Scripps Research Institute
Contact: Press Office – Scripps Research Institute
Image: The image is credited to Scripps
Original Research: Open access.
“Ethanol withdrawal-induced adaptations in prefrontal corticotropin releasing factor receptor 1-expressing neurons regulate anxiety and conditioned rewarding effects of ethanol” by Reesha R. Patel et al. Molecular Psychiatry
Abstract
Ethanol withdrawal-induced adaptations in prefrontal corticotropin releasing factor receptor 1-expressing neurons regulate anxiety and conditioned rewarding effects of ethanol
Prefrontal circuits are thought to underlie aberrant emotion contributing to relapse in abstinence; however, the discrete cell-types and mechanisms remain largely unknown. Corticotropin-releasing factor and its cognate type-1 receptor, a prominent brain stress system, is implicated in anxiety and alcohol use disorder (AUD).
Here, we tested the hypothesis that medial prefrontal cortex CRF1-expressing (mPFCCRF1+) neurons comprise a distinct population that exhibits neuroadaptations following withdrawal from chronic ethanol underlying AUD-related behavior.
We found that mPFCCRF1+ neurons comprise a glutamatergic population with distinct electrophysiological properties and regulate anxiety and conditioned rewarding effects of ethanol.
Notably, mPFCCRF1+ neurons undergo unique neuroadaptations compared to neighboring neurons including a remarkable decrease in excitability and glutamatergic signaling selectively in withdrawal, which is driven in part by the basolateral amygdala.
To gain mechanistic insight into these electrophysiological adaptations, we sequenced the transcriptome of mPFCCRF1+ neurons and found that withdrawal leads to an increase in colony-stimulating factor 1 (CSF1) in this population.
We found that selective overexpression of CSF1 in mPFCCRF1+ neurons is sufficient to decrease glutamate transmission, heighten anxiety, and abolish ethanol reinforcement, providing mechanistic insight into the observed mPFCCRF1+ synaptic adaptations in withdrawal that drive these behavioral phenotypes.
Together, these findings highlight mPFCCRF1+ neurons as a critical site of enduring adaptations that may contribute to the persistent vulnerability to ethanol misuse in abstinence, and CSF1 as a novel target for therapeutic intervention for withdrawal-related negative affect.