Summary: In both healthy people and those with life-threatening infections, the gut microbiome appears to help regulate body temperature.
Source: University of Michigan
What’s considered normal body temperature varies from person to person, yet overall, the average basal temperature of the human body has decreased since the 1860s for unknown reasons. A study points to the gut microbiome as a potential regulator of body temperature, both in health and during life-threatening infections.
The study, led by Robert Dickson, M.D., and his colleagues at U-M Medical School, used health record data from patients hospitalized with sepsis and mouse experiments to examine the interplay between the mix of bacteria residing in the gut, temperature fluctuation, and health outcomes.
Sepsis, the body’s response to a life-threatening infection, can cause drastic changes in body temperature, the trajectory of which is linked to mortality.
Work published in the American Journal of Respiratory and Critical Care Medicine in 2019 has demonstrated that hospitalized patients with sepsis vary widely in their temperature responses, and this variation predicts their survival.
“There’s a reason that temperature is a vital sign,” said Kale Bongers M.D. Ph.D., a clinical instructor in the Department of Internal Medicine and lead author of the study. “It’s both easily measured and tells us important information about the body’s inflammatory and metabolic state.”
Yet the causes of this temperature variation, both in sepsis and in health, have remained unknown.
“We know that temperature response is important in sepsis, because it strongly predicts who lives and who dies,” said Dickson. “But we don’t know what drives this variation and whether it can modified to help patients.”
To try to understand the cause of this variation, the team analyzed rectal swabs from 116 patients admitted to the hospital. The patients’ gut microbiota varied widely, confirming that it is a potential source of variation.
“Arguably, our patients have more variation in their microbiota than they do in their own genetics,” said Bongers. “Any two patients are more than 99% identical in their own genomes, while they may have literally 0% overlap in their gut bacteria.”
The authors found that this variation in gut bacteria was correlated with patient’s temperature trajectories while in the hospital. In particular, common bacteria from the Firmicutes phylum were most strongly associated with increased fever response. These bacteria are common, variable across patients, and are known to produce important metabolites that enter the bloodstream and influence the body’s immune response and metabolism.
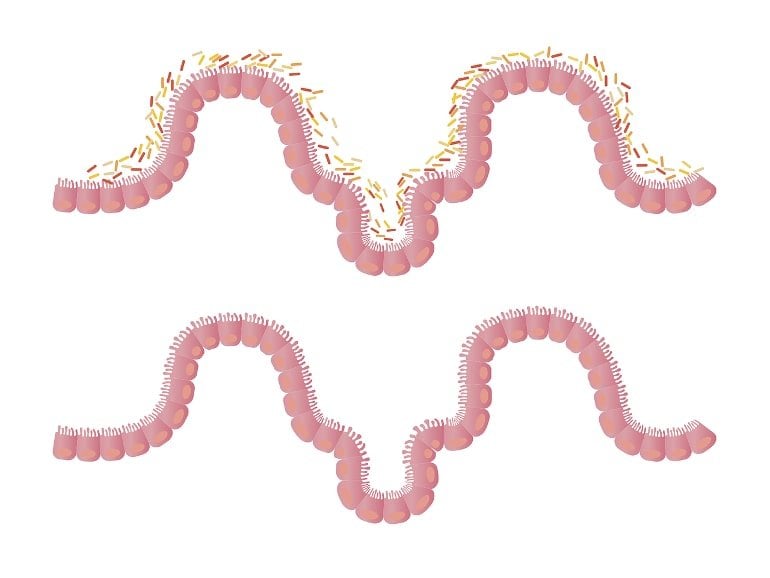
To confirm these findings under controlled conditions, the team used mouse models, comparing normal mice with genetically identical mice that lack a microbiome. Experimental sepsis caused dramatic changes in the temperature of conventional mice but had a blunted effect on the temperature response of germ-free mice. Among mice with a microbiome, variation in temperature response was strongly correlated with the same bacterial family (Lachnospiraceae) that was found in humans.
“We found that the same kind of gut bacteria explained temperature variation both in our human subjects and in our laboratory mice,” said Dickson. “This gave us confidence in the validity of our findings and gives us a target for understanding the biology behind this finding.”
Even in health, mice without a microbiome had lower basal body temperatures than conventional mice. Treating normal mice with antibiotics also reduced their body temperature.
The study highlights an underappreciated role of the gut microbiome in body temperature and could explain the reduction in basal body temperature over the past 150 years.
“While we certainly haven’t proven that changes in the microbiome explain the drop in human body temperature, we think it is a reasonable hypothesis,” said Bongers. “Human genetics haven’t meaningfully changed in the last 150 years, but changes in diet, hygiene, and antibiotics have had profound effects on our gut bacteria.”
Further research is needed to understand whether targeting the microbiome to modulate body temperature could help alter the outcome for patients with sepsis.
About this neuroscience research news
Author: Press Office
Source: University of Michigan
Contact: Press Office – University of Michigan
Image: The image is in the public domain
Original Research: Closed access.
“The Gut Microbiome Modulates Body Temperature Both in Sepsis and Health” by Kale S Bongers et al. American Journal of Respiratory and Critical Care Medicine
Abstract
The Gut Microbiome Modulates Body Temperature Both in Sepsis and Health
Rationale: Among patients with sepsis, variation in temperature trajectories predicts clinical outcomes. In healthy individuals, normal body temperature is variable and has decreased consistently since the 1860s. The biologic underpinnings of this temperature variation in disease and health are unknown.
Objectives: To establish and interrogate the role of the gut microbiome in calibrating body temperature.
Methods: We performed a series of translational analyses and experiments to determine whether and how variation in gut microbiota explains variation in body temperature in sepsis and in health. We studied patient temperature trajectories using electronic medical record data. We characterized gut microbiota in hospitalized patients using 16S ribosomal RNA gene sequencing. We modeled sepsis using intraperitoneal lipopolysaccharide in mice and modulated the microbiome using antibiotics, germ-free, and gnotobiotic animals.
Measurements and main results: Consistent with prior work, we identified four temperature trajectories in patients hospitalized with sepsis that predicted clinical outcomes. In a separate cohort of 116 hospitalized patients, we found that composition of patients’ gut microbiota at admission predicted their temperature trajectories. Compared with conventional mice, germ-free mice had reduced temperature loss during experimental sepsis. Among conventional mice, heterogeneity of temperature response in sepsis was strongly explained by variation in gut microbiota. Healthy germ-free and antibiotic-treated mice both had lower basal body temperatures when compared to controls. The Lachnospiraceae family was consistently associated with temperature trajectories in hospitalized patients, experimental sepsis, and antibiotic-treated mice.
Conclusions: The gut microbiome is a key modulator of body temperature variation both in health and critical illness, and is thus a major, understudied target for modulating physiologic heterogeneity in sepsis.







