Summary: Celiac disease, an autoimmune response to ingesting gluten, has been linked to an increased risk of neurological damage and negative mental health outcomes. Those with celiac disease are more likely to experience depression, anxiety, and thoughts of self-harm, in addition to a reduction in reaction times and cognitive function. Neuroimaging of patients with the disorder reveals white matter changes in the brain.
Source: University of Sheffield
People living with Celiac Disease (CD) have a higher risk of neurological damage according to a new study from the University of Sheffield.
The study found that the brains of people living with CD showed evidence of damage to brain matter and cognitive deficit in the form of slowed reaction times.
Alongside this neurological damage, this group of people also had indications of worsened mental health compared to matched healthy control subjects.
The researchers hope the study will help clinicians to tailor their care to CD patients who may present even the mildest cognitive changes; providing reassurance and motivation for the maintenance of a strict gluten-free diet (GFD), and eradicate any scepticism in the clinical community.
People living with CD have increased sensitivity to gluten and are advised to follow a strict GFD, the only current method of minimising exposure and the immediate risk of damage to their digestive system.
As a result of repeated or uncontrolled exposure, this autoimmune response to gluten can also lead to serious complications and longer term health problems for people living with CD. These include a higher risk of coronary artery disease, small bowel cancers, deterioration of bone health and damage to the nervous system.
There has long been debate amongst neurologists and gastroenterologists about whether this neurological damage is caused as a result of people having CD, with previous studies finding conflicting evidence.
Seeking to end this debate, researchers from the University of Sheffield conducted a study using independent third party study samples from people with no pre-existing neurological illness from the national UK Biobank. This data, including cognitive test scores and brain imaging data was used to eliminate any so-called ‘ascertainment bias’ in their study.
Dr Iain Croall, a research fellow from the University of Sheffield’s Department of Infection, Immunity and Cardiovascular Disease, said and Associate Member of Insigneo: “For the first time, the study offers some clarity on the fact that there does appear to be the risk of neurological damage for people living with CD, driven by their autoimmune response to gluten exposure.
“Our independent UK Biobank participants with CD showed meaningful neurological and psychological deficits when compared with control participants.
“The data from the CD group of participants showed a significant reaction time deficit, compared to the control participants; alongside signs of anxiety, health-related unhappiness and depression.”
Reaction time is an indicator of the cognitive processing speed and people who have compromised white matter tissue frequently show impairments in this area.
Previous research has also highlighted that 50 percent of newly diagnosed CD patients present with clinical neurological symptoms, while population studies have shown living with CD may increase the risk of developing conditions like vascular dementia in older age.
“If previous report findings were due to ascertainment bias, then we would not have found evidence of neuropsychological dysfunction in third party data from the UK Biobank participants,” said Dr Croall.
“What the research shows is that it would be of great benefit for clinicians to support people living with CD to be as vigilant as possible with their gluten-free diet. Reducing any accidental exposure to gluten controls any further brain damage and promotes healing within the digestive system safeguarding a better level of overall health,” said Dr Croall.
Funding: The study was funded by the Sheffield Institute of Gluten Related Disorders, and supported by the National Institute of Health Research (NIHR) Sheffield Biomedical Research Centre and the University of Sheffield Insigneo Institute for in silico Medicine.
The UK Biobank is a valuable international resource that independently holds a wealth of health and demographic data on 500,000 anonymous UK adults, and with consent is made available to health researchers.
Source:
University of Sheffield
Media Contacts:
Rebecca Ferguson – University of Sheffield
Image Source:
The image is credited to Iain Croall et al.
Original Research: Closed access
“Cognitive Deficit and White Matter Changes in Persons with Celiac Disease: a Population-Based Study”. Iain Croall et al.
Gastroenterology doi:10.1053/j.gastro.2020.02.028.
Abstract
Cognitive Deficit and White Matter Changes in Persons with Celiac Disease: a Population-Based Study
Background & Aims
There is debate over the presence and prevalence of brain injury in patients with celiac disease. To validate previous reports, we investigated the prevalence of neuropsychological dysfunction in persons with celiac disease included in the National UK Biobank, which contains experimental medical data from 500,000 adults in the United Kingdom.
Methods
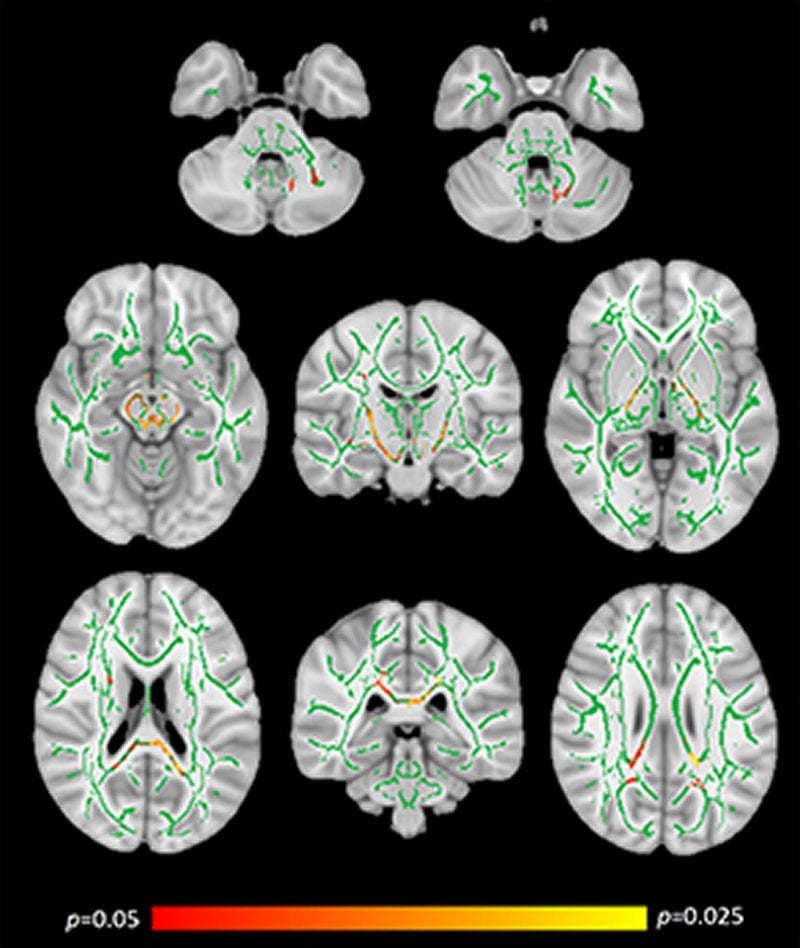
Biobank participants with celiac disease (n=104; mean age, 63; 65% female) were matched with healthy individuals (controls, n=198; mean age, 63 y; 67% female) for age, sex, level of education, body mass index, and diagnosis of hypertension. All subjects were otherwise healthy. We compared scores from 5 cognitive tests, and multiple-choice responses to 6 questions about mental health, between groups using t test and χ2 analyses. Groupwise analyses of magnetic resonance imaging brain data included a study of diffusion tensor imaging metrics (mean diffusivity, fractional anisotropy, radial diffusivity, axial diffusivity), voxel-based morphometry, and Mann-Whitney U comparisons of Fazekas grades.
Results
Compared with controls, participants with celiac disease had significant deficits in reaction time (P=.004) and significantly higher proportions had indications of anxiety (P=.025), depression (P=.015), thoughts of self-harm (P=.025) and health-related unhappiness (P=.010). Tract-based spatial statistics analysis revealed significantly increased axial diffusivity in widespread locations, demonstrating white matter changes in brains of participants with celiac disease. Voxel-based morphometry and Fazekas grade analyses did not differ significantly between groups.
Conclusions
In an analysis of data from the UK Biobank, we found participants with celiac disease to have cognitive deficit, indications of worsened mental health, and white matter changes, based on analyses of brain images. These findings support the concept that celiac disease is associated with neurological and psychological features.






