Summary: A new study reveals a genetic link between Alzheimer’s disease and several gut-related disorders. Researchers report Alzheimer’s patients and those with intestinal disorders have specific genes in common. The findings add to the evidence the gut-brain axis may play a role in the development of neurodegenerative disorders.
Source: Edith Cowan University
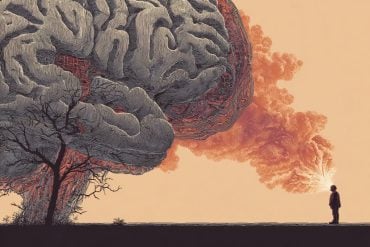
People with gut disorders may be at greater risk of developing Alzheimer’s Disease (AD).
A world-first Edith Cowan University (ECU) study has confirmed the link between the two, which could lead to earlier detection and new potential treatments.
AD destroys memory and thinking ability and is the most prevalent form of dementia.
It has no known curative treatments and is expected to affect more than 82 million people and cost US$2 trillion by 2030.
Previous observational studies have suggested a relationship between AD and gastrointestinal tract disorders, but what underpins these relationships had been unclear – until now.
ECU’s Centre for Precision Health has now provided new insights into these relationships by confirming a genetic link between AD and multiple gut disorders.
The study analysed large sets of genetic data from AD and several gut-disorder studies – each of about 400,000 people.
Research lead Dr Emmanuel Adewuyi said it was the first comprehensive assessment of the genetic relationship between AD and multiple gut disorders.
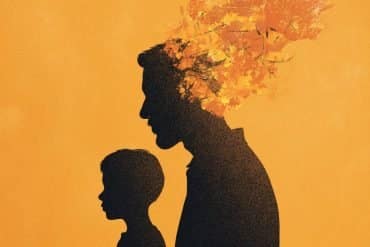
The team discovered people with AD and gut disorders have genes in common – which is important for many reasons.
“The study provides a novel insight into the genetics behind the observed co-occurrence of AD and gut disorders,” Dr Adewuyi said.
“This improves our understanding of the causes of these conditions and identifies new targets to investigate to potentially detect the disease earlier and develop new treatments for both types of conditions.”
Centre for Precision Health director and study supervisor Professor Simon Laws said whilst the study didn’t conclude gut disorders cause AD or vice versa, the results are immensely valuable.
“These findings provide further evidence to support the concept of the ‘gut-brain’ axis, a two-way link between the brain’s cognitive and emotional centres, and the functioning of the intestines,” Professor Laws said.
Is cholesterol a key?
When researchers conducted further analysis into the shared genetics, they found other important links between AD and gut disorders – such as the role cholesterol may play.
Dr Adewuyi said abnormal levels of cholesterol were shown to be a risk for both AD and gut disorders.
“Looking at the genetic and biological characteristics common to AD and these gut disorders suggests a strong role for lipids metabolism, the immune system, and cholesterol-lowering medications,” he said.

“Whilst further study is needed into the shared mechanisms between the conditions, there is evidence high cholesterol can transfer into the central nervous system, resulting in abnormal cholesterol metabolism in the brain.
“There is also evidence suggesting abnormal blood lipids may be caused or made worse by gut bacteria (H.pylori), all of which support the potential roles of abnormal lipids in AD and gut disorders.
“For example, elevated cholesterol in the brain has been linked to brain degeneration and subsequent cognitive impairment.”
Hope for the future
The cholesterol link could prove vital in treating AD in the future.
While there are currently no known curative treatments, the study’s findings suggest cholesterol lowering medications (statins) could be therapeutically beneficial in treating both AD and gut disorders.
“Evidence indicates statins have properties which help reduce inflammation, modulate immunity and protect the gut,” Dr Adewuyi said.
However, he said there was a need for more studies and patients needed to be assessed individually to judge whether they would benefit from statin use.
The research also indicated diet could play a part in treating and preventing AD and gut disorders.
About this Alzheimer’s disease and genetics research news
Author: Sam Jeremic
Source: Edith Cowan University
Contact: Sam Jeremic – Edith Cowan University
Image: The image is credited to Edith Cowan University
Original Research: Open access.
“A large-scale genome-wide cross trait analysis reveals shared genetic architecture between Alzheimer’s disease and gastrointestinal tract disorders” by Simon Laws et al. Communications Biology
Abstract
A large-scale genome-wide cross trait analysis reveals shared genetic architecture between Alzheimer’s disease and gastrointestinal tract disorders
Consistent with the concept of the gut-brain phenomenon, observational studies suggest a relationship between Alzheimer’s disease (AD) and gastrointestinal tract (GIT) disorders; however, their underlying mechanisms remain unclear.
Here, we analyse several genome-wide association studies (GWAS) summary statistics (N = 34,652–456,327), to assess the relationship of AD with GIT disorders. Findings reveal a positive significant genetic overlap and correlation between AD and gastroesophageal reflux disease (GERD), peptic ulcer disease (PUD), gastritis-duodenitis, irritable bowel syndrome and diverticulosis, but not inflammatory bowel disease.
Cross-trait meta-analysis identifies several loci (Pmeta-analysis < 5 × 10−8) shared by AD and GIT disorders (GERD and PUD) including PDE4B, BRINP3, ATG16L1, SEMA3F, HLA-DRA, SCARA3, MTSS2, PHB, and TOMM40. Colocalization and gene-based analyses reinforce these loci. Pathway-based analyses demonstrate significant enrichment of lipid metabolism, autoimmunity, lipase inhibitors, PD-1 signalling, and statin mechanisms, among others, for AD and GIT traits.
Our findings provide genetic insights into the gut-brain relationship, implicating shared but non-causal genetic susceptibility of GIT disorders with AD’s risk.
Genes and biological pathways identified are potential targets for further investigation in AD, GIT disorders, and their comorbidity.