Summary: A new study in mice shows that briefly anesthetizing the retina of the weaker eye can restore its neural influence in the adult visual cortex. The treatment activates a specific burst-firing mode in thalamic neurons, a developmental mechanism that reopens plasticity even after the usual critical period has closed.
Importantly, the effect arises when either eye is inactivated, suggesting that direct treatment of the weaker eye may restore vision without disrupting the stronger one. These findings point to a promising path toward adult amblyopia therapies that were previously thought impossible.
Key Facts
- Reversible Retina Silencing: Temporarily anesthetizing the amblyopic eye reactivates its visual pathways even in adulthood.
- Burst Activity Is Essential: Restorative effects depend on T-type calcium channel–mediated bursting in thalamic relay neurons.
- Potential New Therapy: The approach may allow treatment of amblyopia without blocking the stronger eye, pending future validation.
Source: Picower Institute at MIT
In the common vision disorder amblyopia, impaired vision in one eye during development causes neural connections in the brain’s visual system to shift toward supporting the other eye, leaving the amblyopic eye less capable even after the original impairment is corrected.
Current interventions are only effective during infancy and early childhood while the neural connections are still being formed.
But a new study in mice by neuroscientists in The Picower Institute for Learning and Memory at MIT shows that if the retina of the amblyopic eye is temporarily and reversibly anesthetized just for a couple of days, the brain’s visual response to the eye can be restored even in adulthood.
The findings, published in Cell Reports, may improve the clinical potential of the idea of temporarily anesthetizing a retina to restore the strength of the amblyopic eye’s neural connections.
In 2021 the lab of Picower Professor Mark Bear and collaborators showed that anesthetizing the non-amblyopic eye could improve vision in the amblyopic one—an approach analogous in that way to the treatment used in childhood of patching the unimpaired eye.
That 2021 findings have now been replicated in adults of multiple species. But the new evidence on how inactivation works suggests that the proposed treatment also could be effective when applied directly to the amblyopic eye, Bear said, though a key next step will be to again show that it works in additional species and, ultimately, people.
“If it does, it’s a pretty substantial step forward because it would be reassuring to know that vision in the good eye would not have to be interrupted by treatment,” said Bear, a faculty member in MIT’s Department of Brain and Cognitive Sciences.
“The amblyopic eye, which is not doing much, could be inactivated and ‘brought back to life’ instead. Still, I think that especially with any invasive treatment, it’s extremely important to confirm the results in higher species with visual systems closer to our own.”
Madison Echavarri-Leet, a former graduate student whose doctoral thesis included this research, is the lead author of the study, which also demonstrates the underlying process in the brain that makes the potential treatment work.
A beneficial burst
Bear’s lab has been studying the science underlying amblyopia for decades, for instance by working to understand the molecular mechanisms that enable neural circuits to change their connections in response to visual experience or deprivation. The research has produced ideas about how to address amblyopia in adulthood.
In a 2016 study with collaborators at Dalhousie University they showed that temporarily anesthetizing both retinas could restore vision loss in amblyopia. Then five years later, they published the study showing that anesthetizing just the non-amblyopic eye produced visual recovery for the amblyopic eye.
Throughout that time, the lab weighed multiple hypotheses to explain how retinal inactivation works its magic. Lingering in the lab’s archive of results, Bear said, was an unexplored finding in the lateral geniculate nucleus (LGN) that relays information from the eyes to the visual cortex, where vision is processed: Back in 2008 they had found that blocking inputs from a retina to neurons in the LGN caused those neurons to fire synchronous “bursts” of electrical signals to downstream neurons in the visual cortex.
Similar patterns of activity occur in the visual system before birth and guide early synaptic development.
The new study tested whether those bursts might have a role in the potential amblyopia treatments the lab was reporting. To get started, Leet and Bear’s team used a single injection of tetrodotoxin (TTX) to anesthetize retinas in the lab animals. They found that the bursting occurred not only in LGN neurons that received input from the anesthetized eye, but also in LGN neurons that received input from the unaffected eye.
From there they showed that the bursting response depended on a particular “T-type” channel for calcium in the LGN neurons. This was important because knowing this gave the scientists a way to turn it off. Once they gained that ability, then they could test whether doing so prevented TTX from having a therapeutic effect in mice with amblyopia.
Sure enough, when the researchers genetically knocked out the channels and disrupted the bursting, they found that anesthetizing the non-amblyopic eye could no longer help amblyopic mice. That showed the bursting is necessary for the treatment to work.
Aiding amblyopia
Given their finding that bursting occurs when either retina is anesthetized, the scientists hypothesized it might be enough to just do it in the amblyopic eye. To test this, they ran an experiment in which some mice modeling amblyopia received TTX in their amblyopic eye and some did not.
The injection took the retina offline for two days. After a week the scientists then measured activity in neurons in the visual cortex to calculate a ratio of input from each eye.
They found that the ratio was much more even in mice that received the treatment vs. those left untreated, indicating that after the amblyopic eye was anesthetized, its input in the brain rose to be at parity with input from the non-amblyopic one.
Further testing is needed, Bear notes, but the team wrote in the study that the results were encouraging.
“We are cautiously optimistic that these findings may lead to a new treatment approach for human amblyopia, particularly given the discovery that silencing the amblyopic eye is effective,” the scientists wrote.
In addition to Leet and Bear, the paper’s authors are Tushar Chauhan, Teresa Cramer and Ming-fai Fong.
Funding: The National Institutes of Health, the Swiss National Science Foundation, the Severin Hacker Vision Research Fund and the Freedom Together Foundation supported the study.
Key Questions Answered:
A: Temporarily silencing the retina triggers restorative neural bursting that strengthens the amblyopic eye’s pathways.
A: Instead of blocking the stronger eye, this method directly revives the weaker eye’s neural connections.
A: Burst activity in thalamic relay neurons drives plasticity that rebalances visual input between both eyes.
Editorial Notes:
- This article was edited by a Neuroscience News editor.
- Journal paper reviewed in full.
- Additional context added by our staff.
About this visual neuroscience research news
Author: David Orenstein
Source: Picower Institute at MIT
Contact: David Orenstein – Picower Institute at MIT
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Temporary retinal inactivation reverses effects of long-term monocular deprivation in visual cortex by induction of burst mode firing in the thalamus” by Mark Bear et al. Cell Reports
Abstract
Temporary retinal inactivation reverses effects of long-term monocular deprivation in visual cortex by induction of burst mode firing in the thalamus
Monocular deprivation during an early postnatal critical period causes amblyopia, an impairment of vision in one eye, by altering the development of synapses in the primary visual cortex (V1).
Prior studies have shown that these synaptic changes can be rapidly reversed after the critical period by temporarily inactivating the non-deprived (fellow) eye with tetrodotoxin (TTX).
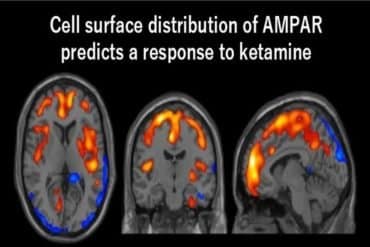
Here, we show in mice that the inactivation of one eye causes dorsal lateral geniculate nucleus (dLGN) neurons postsynaptic to the other eye to fire in high-frequency bursts due to recruitment of the low-threshold voltage-gated calcium channels.
Elimination of bursting by genetic deletion of CaV3.1 in the dLGN prevents the therapeutic effect of retinal inactivation without affecting another prominent form of experience-dependent synaptic modification.
Inactivation of the amblyopic eye alone also triggered full recovery, suggesting that dLGN bursting is both necessary and sufficient to restore synaptic strength in the visual cortex after retinal silencing.