Summary: New research uncovers how tau pathology spreads and damages synapses in progressive supranuclear palsy (PSP). Using human postmortem tissue and live brain slice models, scientists showed tau accumulates in both pre- and postsynaptic terminals, likely propagating neuron-to-neuron.
Tau-containing synapses were more likely to be lost, and reactive astrocytes were observed engulfing tau-laden synapses. The findings highlight synaptic tau as a key driver of PSP and a promising therapeutic target.
Key Facts
- Synaptic Tau Spread: Tau accumulates in both sides of the synapse, suggesting neuron-to-neuron transmission through synaptic connections.
- Astrocytic Engulfment: Reactive astrocytes engulf tau-laden synapses, contributing to synapse loss.
- Therapeutic Implications: Targeting synaptic tau may slow PSP progression and preserve neuronal circuits.
Source: Neuroscience News
Progressive supranuclear palsy (PSP) is a devastating neurodegenerative disease that robs people of balance, movement, and cognition, progressing relentlessly over time. At the heart of this condition lies tau—a protein that, when it becomes misfolded and aggregated, spreads throughout the brain.
While researchers have long known that tau pathology and synapse loss go hand in hand, exactly how tau damages synapses and propagates between neurons has remained a mystery.
Now, an innovative new study offers critical insights, showing that tau directly infiltrates synapses, disrupts their function, and even recruits astrocytes—the brain’s support cells—to destroy them.
This research, combining postmortem human brain samples and live human brain slice models, not only confirms tau’s presence in both pre- and postsynaptic terminals but also suggests that tau spreads neuron-to-neuron through these synaptic connections. These findings point to synaptic tau as a key target for future therapies, raising hope for slowing or even halting PSP progression.
The Curious Case of Tau
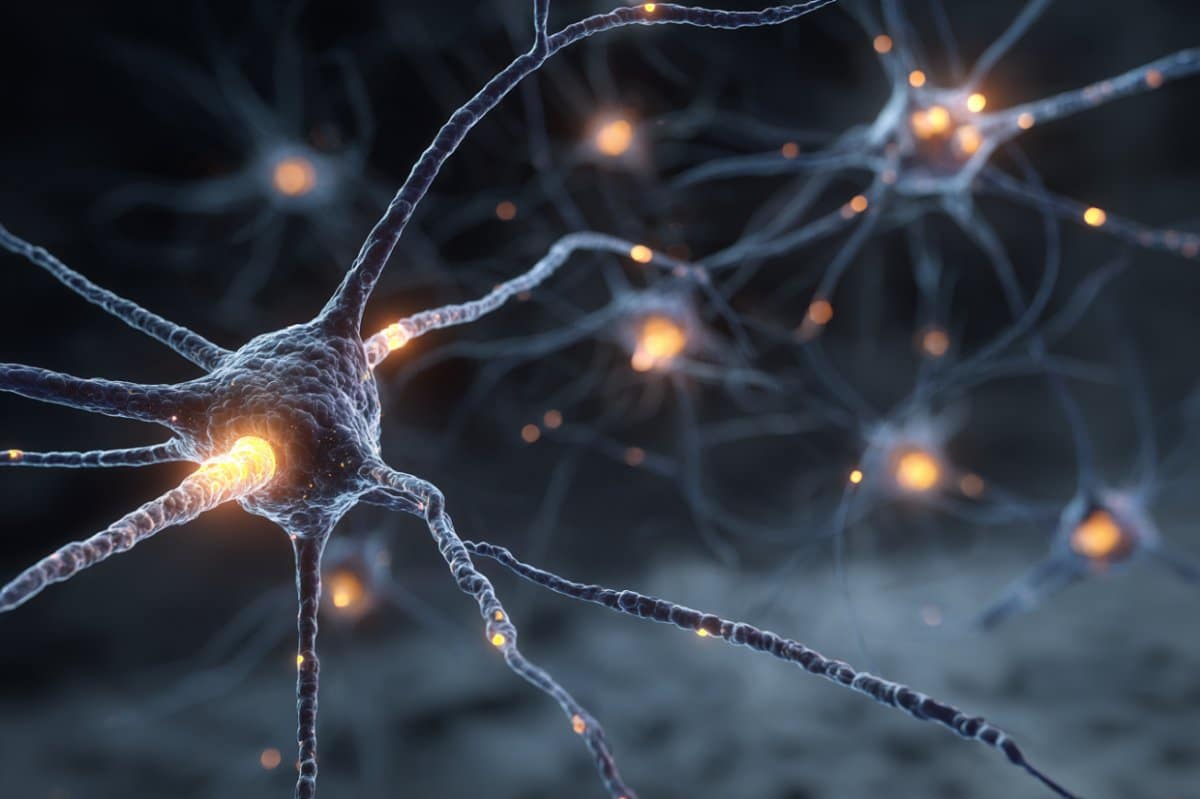
Tau is best known as the structural protein stabilizing microtubules within neurons. But in diseases like PSP and Alzheimer’s, tau becomes hyperphosphorylated and forms aggregates that disrupt neurons and eventually kill them.
In PSP, tau pathology progresses in a predictable pattern across brain regions, and regions with more tau show worse synapse loss and more severe symptoms.
The question has been: does tau just appear where damage is already occurring, or is it actively spreading through connections and causing that damage? To answer this, researchers turned their attention to the most intimate sites of neuron-to-neuron communication: synapses.
Tau Invades Synaptic Pairs
In the study, scientists examined postmortem brains from people with PSP, using advanced imaging techniques to look at synapses. They found clear evidence that tau, particularly its toxic oligomeric form, accumulates not just on one side of a synapse but often in both the presynaptic terminal and the opposing postsynapse.
Remarkably, postsynapses were over 80 times more likely to contain tau if paired with a tau-containing presynapse—strongly suggesting trans-synaptic propagation.
Super-resolution imaging also showed that tau closely associates with synaptic proteins like synaptogyrin-3, supporting earlier animal studies that linked tau-synaptic protein interactions to dysfunction. Importantly, synapses containing tau were more likely to be lost, revealing tau’s direct toxicity at the synaptic level.
Astrocytes Join the Attack
The researchers didn’t stop there. They also investigated whether glial cells—particularly astrocytes—might be complicit in synaptic loss. In PSP brains, astrocytes were more reactive and engulfed more synapses than in healthy controls. Strikingly, many of the synapses astrocytes consumed contained tau.
This suggests that astrocytes may detect tau-containing synapses as “damaged” and remove them, perhaps as a misguided attempt to protect the network—one that ends up worsening the disease.
A Living Human Brain Slice Model
To confirm that tau can infiltrate postsynapses and drive astrocytic responses in living tissue, the team developed an innovative model: slices of live human cortex obtained during surgical procedures.
When exposed to soluble tau extracted from PSP brains, these slices quickly showed tau accumulating in postsynaptic terminals and astrocytes becoming reactive and engulfing more synapses—recapitulating what was observed in postmortem tissue.
This is a critical advance, proving that human synapses can actively take up pathological tau and that the phenomenon isn’t merely a byproduct of cell death.
Clusterin: A New Accomplice?
One unexpected finding was the role of clusterin, a protein previously implicated in Alzheimer’s disease. Clusterin levels were elevated in PSP synapses and found to physically interact with tau in postsynaptic terminals.
This raises the intriguing possibility that clusterin helps shuttle tau into synapses—or perhaps facilitates its toxicity there. This new target warrants further investigation as a possible therapeutic lever.
Why This Matters
The study’s implications are profound. By establishing that tau spreads through synaptic connections, damages synapses directly, and recruits astrocytes to destroy them, it pinpoints synaptic tau as a key mediator of PSP progression.
Therapies that block tau’s entry into synapses or its toxic interactions there could help preserve neuronal circuits. In fact, monoclonal antibodies targeting synaptic tau oligomers are already being explored in clinical trials.
Moreover, the findings reveal that PSP may not only involve irreversible damage but also dynamic processes that could be modified—offering hope to patients facing this currently untreatable disease.
Looking Ahead
The research opens new questions. Why do some synapses seem more vulnerable to tau? Could targeting astrocytic overactivity reduce synaptic loss? And does the same synaptic tau mechanism underlie related tauopathies like Alzheimer’s and frontotemporal dementia?
Future studies will likely explore these avenues, aiming to transform our understanding of neurodegenerative diseases and move toward therapies that protect the most critical nodes of brain communication: synapses.
By bringing the hidden story of synaptic tau into the spotlight, this research underscores the importance of looking beyond neurons to the connections between them—and the glial cells that police those connections. In the battle against PSP, synapses may prove to be both the battleground and the key to victory.
About this PSP and neurology research news
Author: Neuroscience News Communications
Source: Neuroscience News
Contact: Neuroscience News Communications – Neuroscience News
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Evidence for trans-synaptic propagation of oligomeric tau in human progressive supranuclear palsy” by Robert I. McGeachan et al. Nature Neuroscience
Abstract
Evidence for trans-synaptic propagation of oligomeric tau in human progressive supranuclear palsy
In the neurodegenerative disease progressive supranuclear palsy (PSP), tau pathology progresses through the brain in a stereotypical spatiotemporal pattern, and where tau pathology appears, synapses are lost.
We tested the hypothesis that pathological tau contributes to synapse loss and may spread through the brain by moving from presynapses to postsynapses.
Using postmortem PSP brain samples and a living human brain slice culture model, we observe pathological tau in synaptic pairs and evidence that oligomeric tau can enter live human postsynapses.
Proteomics revealed increased clusterin in synapses in PSP, and super-resolution imaging showed clusterin colocalized with tau in synapses in close enough proximity to be binding partners, which may mediate tau spread.
Accumulation of tau in synapses correlated with synapse loss, and synaptic engulfment by astrocytes was observed, suggesting that astrocytes contribute to synapse loss.
Together, these data indicate that targeting synaptic tau is a promising approach to treat PSP.