By studying specially bred mice with specific developmental and cognitive traits resembling those seen in schizophrenia, UC San Francisco researchers have provided new evidence that abnormal rhythmic activity in particular brain cells contributes to problems with learning, attention, and decision-making in individuals with that disorder.
As reported in the March 5, 2015 online edition of Neuron, when the researchers corrected these cells’ faulty rhythm, either by directly stimulating the cells or by administering low doses of a commonly used drug, cognitive deficits in the mice were reversed, results that point the way to possible therapies to address cognitive symptoms in individuals with schizophrenia.
According to Vikaas Sohal, MD, PhD, senior author of the new study, in addition to dealing with the burdens of schizophrenia’s so-called positive symptoms (such as delusions and hallucinations) and negative symptoms (such as social withdrawal and a lack of motivation), individuals with the disorder also grapple with cognitive deficits that create considerable challenges in the arenas of education, work, and interpersonal relationships.
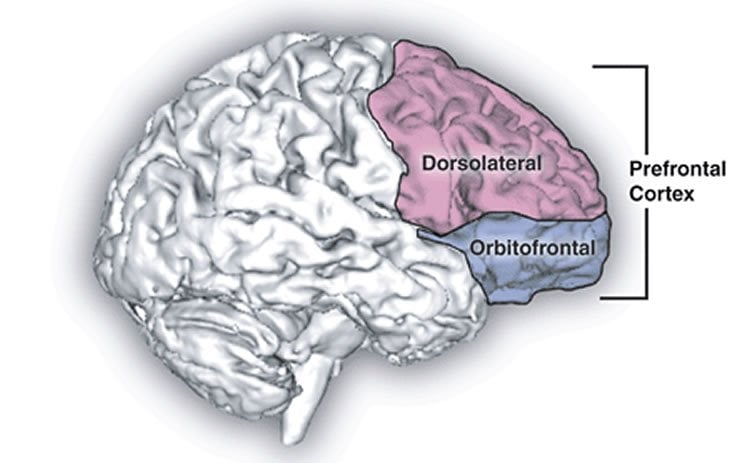
Converging evidence from many previous studies has implicated a population of neurons in the brain’s prefrontal cortex called fast-spiking (FS) interneurons in schizophrenia, but a causal relationship between malfunctioning FS interneurons and cognitive symptoms of the disorder has not yet been firmly established, Sohal said.
For example, individuals with schizophrenia perform poorly on the Wisconsin Card-Sorting Test (WSCT), an assessment tool designed more than 60 years ago that sensitively measures the ability to learn new rules on the fly and apply them to complete a task.
Electroencephalography (“brain wave”) studies of normal individuals have revealed that gamma oscillations—neural activity with a regular rhythm between 30 and 120 cycles per second—increase in the front of the brain during cognitive tasks related to the WCST, but “these gamma oscillations are blunted in individuals with schizophrenia,” said Sohal, the Staglin Family-IMHRO Assistant Professor of Psychiatry at UCSF.
Because gamma oscillations emerge from the activity of FS interneurons, and because postmortem studies of the brains of individuals with schizophrenia have shown biochemical abnormalities in FS interneurons, many researchers have concluded these neurons must play some role in the cognitive symptoms of the disorder.
In the new research, first author and postdoctoral fellow Kathleen K.A. Cho, PhD, led a team that made use of mice developed in the UCSF laboratory of John L.R. Rubenstein, MD, PhD, the Nina Ireland Distinguished Professor in Child Psychiatry. These mice carry only one copy of two genes known as Dlx5 and Dlx6, which govern the proper assembly of FS interneuron circuitry as the brain develops. An intriguing characteristic of these mice is that FS interneurons only become abnormal at a developmental stage corresponding to human post-adolescence, which is when symptoms of schizophrenia usually begin to emerge.
In the new research when these mice performed a “rule-shift” task—designed to emulate important features of the WCST—at a young age, their performance was indistinguishable from that of normal mice. But they showed significant deficits when they performed the task as young adults.
To firmly establish that interneuron abnormalities were responsible for this declining performance, the researchers disrupted gamma oscillations in normal adult mice with a technique that allowed them to shine a light into the brain to inhibit the activity of interneurons in the prefrontal cortex, including FS interneurons. These mice performed as poorly on the rule-shift task as those lacking Dlx5 and Dlx6.
Conversely, the scientists used a similar technique to restore gamma oscillations by stimulating interneurons in the prefrontal cortex with light in mice lacking Dlx5 and Dlx6, and the mice performed the task as well as normal mice.
Finally, when the team gave low doses of clonazepam (Klonopin), which modulates the GABA neurotransmitter system employed by FS interneurons, to mice lacking Dlx5 and Dlx6, the mice again performed the rule-shifting task normally.
The cognitive improvements following direct interneuron stimulation persisted for a week after the experiments, suggesting that targeting FS interneuron dysfunction may result in durable improvements in cognitive function in schizophrenia.
Clonazepam and other GABA-modulating drugs such as lorazepam (Ativan) and diazepam (Valium) are now used to treat anxiety associated with schizophrenia, but usually at higher doses that also increase sedation, which may mask any cognition-enhancing effect. Lower doses, or better-designed compounds that specifically target FS interneurons in the prefrontal cortex, might be better options, Sohal said, adding that measuring gamma oscillations may be a useful guide in developing these approaches.
On a more speculative level, Sohal added, it may be possible to increase gamma oscillations to improve cognition using recently developed, non-invasive brain stimulation technologies such as transcranial magnetic or direct-current stimulation (TMS or tDCS), or even by combining meditation with biofeedback.
“Meditation has been shown to potently increase gamma oscillations, and you may be able to teach patients to increase gamma oscillations by themselves,” said Sohal. “Now that we know that gamma oscillations are directly related to cognitive performance, it’s certainly an interesting idea to pursue.”
In addition to Sohal, Cho, and Rubenstein, researchers participating in the study included former postdoctoral fellow Renee Hoch, PhD; Anthony Lee, a student in USCF’s MD/PhD program; and laboratory specialist Tosha Patel.
The work was supported by the Staglin Family and the International Mental Health Research Organization; the National Institute of Mental Health; the Alfred P. Sloan Foundation; the National Institutes of Health; and the Brain and Behavior Research Foundation.
Contact: Pete Farley – UCSF
Source: UCSF press release
Image Source: The image is credited to Natalie M. Zahr, Ph.D., and Edith V. Sullivan, Ph.D./NIH and is in the public domain
Original Research: Abstract for “Gamma Rhythms Link Prefrontal Interneuron Dysfunction with Cognitive Inflexibility in Dlx5/6+/− Mice” by Kathleen K.A. Cho, Renee Hoch, Anthony T. Lee, Tosha Patel, John L.R. Rubenstein, and Vikaas S. Sohal in Neuron. Published online March 5 2015 doi:10.1016/j.neuron.2015.02.019