Scientists have discovered that a commonly prescribed dementia drug could hold the key to helping prevent debilitating falls for people with Parkinson’s.
The research, published today in The Lancet Neurology, shows people with Parkinson’s who were given the oral drug rivastigmine were 45% less likely to fall and were considerably steadier when walking, compared to those on the placebo.
Parkinson’s affects 127,000 people in the UK and approximately seven million worldwide. 70% of people with Parkinson’s will fall at least once a year, with over a third experiencing falls repeatedly, resulting in fractures, broken bones and hospital admissions.
Parkinson’s UK Research Fellow Dr Emily Henderson and principal researcher on the study, based at the University of Bristol, said:
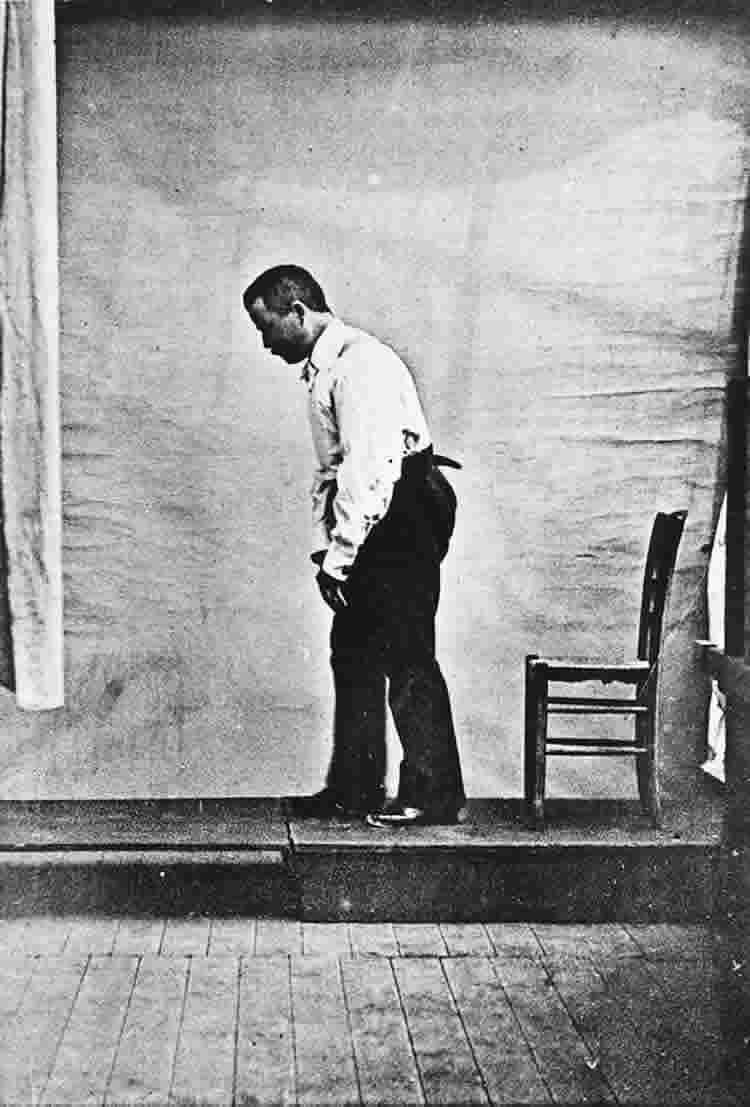
“With the degeneration of dopamine producing nerve cells, people with Parkinson’s often have issues with unsteadiness when walking. As part of the condition, they also have lower levels of acetylcholine, a chemical which helps us to concentrate – making it extremely difficult to pay attention to walking.
“We already know that rivastigmine works to treat dementia by preventing the breakdown of acetylcholine, however our study shows for the first time that it can also improve regularity of walking, speed, and balance. This is a real breakthrough in reducing the risk of falls for people with Parkinson’s.”
Dr Henderson and her team at the University of Bristol studied 130 people with Parkinson’s who had fallen in the past year. Half the group were given rivastigmine capsules and the other half a placebo for an eight month period.
Dr Arthur Roach, Director of Research at Parkinson’s UK, which funded the study said:
“People affected by Parkinson’s, their carers, and health and social care professionals have said that preventing falls and improving balance is the biggest unmet need for people living with the condition, other than finding a cure.
“Things that may be simple to us, such as walking upstairs or getting up in the middle of the night to get a glass of water, or go to the toilet, are much harder and more dangerous when you could easily fall. You risk breaking bones and then needing an emergency hospital admission.
“This trial shows that there may be drugs already available, being used for other purposes, that can be tested to help treat Parkinson’s. This takes us a step closer to improving the quality of life and finding better treatments for people with Parkinson’s.”
Caroline Maxwell from Northamptonshire, a participant on the study, who was diagnosed with Parkinson’s 13 years ago said:
“A few years ago, I had a bad fall while carrying my sewing machine across the room, leaving me in hospital for a week and really denting my confidence.
Emily Henderson talks about the results of her groundbreaking clinical trial. The results suggest that a drug previously used for dementia could help to prevent falls in Parkinson’s patients.
“I’m at the stage where I would walk much better with a replacement joint, but because I fall so frequently my surgeon is reluctant to operate. Falling on my replacement hip would put in an even worse situation than what I’m in now.
“By potentially finding a treatment that helps to prevent falls, I’d be able to get a replacement hip and have the confidence to go shopping on my own, without having to constantly rely on the goodness of strangers to pick me up when I fell.”
Funding: Funding was provided by Parkinson’s UK.
Source: Hanna Kilpin – Parkinson’s UK
Image Source: The image is in the public domain
Video Source: The video is available at the Parkinson’s UK YouTube page
Original Research: Full open access research for for “Rivastigmine for gait stability in patients with Parkinson’s disease (ReSPonD): a randomised, double-blind, placebo-controlled, phase 2 trial” by Emily J Henderson, Stephen R Lord, Matthew A Brodie, Daisy M Gaunt, Andrew D Lawrence, Jacqueline C T Close, A L Whone, and Y Ben-Shlomo in Lancet Neurology. Published online January 12 2016 doi:10.1016/S1474-4422(15)00389-0
Abstract
Rivastigmine for gait stability in patients with Parkinson’s disease (ReSPonD): a randomised, double-blind, placebo-controlled, phase 2 trial
Background
Falls are a frequent and serious complication of Parkinson’s disease and are related partly to an underlying cholinergic deficit that contributes to gait and cognitive dysfunction in these patients. Gait dysfunction can lead to an increased variability of gait from one step to another, raising the likelihood of falls. In the ReSPonD trial we aimed to assess whether ameliorating this cholinergic deficit with the acetylcholinesterase inhibitor rivastigmine would reduce gait variability.
Methods
We did this randomised, double-blind, placebo-controlled, phase 2 trial at the North Bristol NHS Trust Hospital, Bristol, UK, in patients with Parkinson’s disease recruited from community and hospital settings in the UK. We included patients who had fallen at least once in the year before enrolment, were able to walk 18 m without an aid, had no previous exposure to an acetylcholinesterase inhibitor, and did not have dementia. Our clinical trials unit randomly assigned (1:1) patients to oral rivastigmine or placebo capsules (both taken twice a day) using a computer-generated randomisation sequence and web-based allocation. Rivastigmine was uptitrated from 3 mg per day to the target dose of 12 mg per day over 12 weeks. Both the trial team and patients were masked to treatment allocation. Masking was achieved with matched placebo capsules and a dummy uptitration schedule. The primary endpoint was difference in step time variability between the two groups at 32 weeks, adjusted for baseline age, cognition, step time variability, and number of falls in the previous year. We measured step time variability with a triaxial accelerometer during an 18 m walking task in three conditions: normal walking, simple dual task with phonemic verbal fluency (walking while naming words beginning with a single letter), and complex dual task switching with phonemic verbal fluency (walking while naming words, alternating between two letters of the alphabet). Analysis was by modified intention to treat; we excluded from the primary analysis patients who withdrew, died, or did not attend the 32 week assessment. This trial is registered with ISRCTN, number 19880883.
Findings
Between Oct 4, 2012 and March 28, 2013, we enrolled 130 patients and randomly assigned 65 to the rivastigmine group and 65 to the placebo group. At week 32, compared with patients assigned to placebo (59 assessed), those assigned to rivastigmine (55 assessed) had improved step time variability for normal walking (ratio of geometric means 0·72, 95% CI 0·58–0·88; p=0·002) and the simple dual task (0·79; 0·62–0·99; p=0·045). Improvements in step time variability for the complex dual task did not differ between groups (0·81, 0·60–1·09; p=0·17). Gastrointestinal side-effects were more common in the rivastigmine group than in the placebo group (p<0·0001); 20 (31%) patients in the rivastigmine group versus three (5%) in the placebo group had nausea and 15 (17%) versus three (5%) had vomiting.
Interpretation
Rivastigmine can improve gait stability and might reduce the frequency of falls. A phase 3 study is needed to confirm these findings and show cost-effectiveness of rivastigmine treatment.
Funding
Parkinson’s UK.
“Rivastigmine for gait stability in patients with Parkinson’s disease (ReSPonD): a randomised, double-blind, placebo-controlled, phase 2 trial” by Emily J Henderson, Stephen R Lord, Matthew A Brodie, Daisy M Gaunt, Andrew D Lawrence, Jacqueline C T Close, A L Whone, and Y Ben-Shlomo in Lancet Neurology. Published online January 12 2016 doi:10.1016/S1474-4422(15)00389-0






