Summary: Researchers have developed new neural implants that enable targeted delivery of drugs deep into brain structures.
Source: MIT.
The diversity of structures and functions of the brain is becoming increasingly realized in research today. Key structures exist in the brain that regulate emotion, anxiety, happiness, memory, and mobility. These structures can come in a huge variety of shapes and sizes and can all be physically near one another. Dysfunction of these structures and circuits linking them are common causes of many neurologic and neuropsychiatric diseases. For example, the substantia nigra is only a few millimeters in size yet is crucial for movement and coordination. Destruction of substantia nigra neurons is what causes motor symptoms in Parkinson’s disease.
New technologies such as optogenetics have allowed us to identify similar microstructures in the brain. However, these techniques rely on liquid infusions into the brain, which prepare the regions to be studied to respond to light. These infusions are done with large needles, which do not have the fine control to target specific regions. Clinical therapy has also lagged behind. New drug therapies aimed at treating these conditions are delivered orally, which results in drug distribution throughout the brain, or through large needle-cannulas, which do not have the fine control to accurately dose specific regions. As a result, patients of neurologic and psychiatric disorders frequently fail to respond to therapies due to poor drug delivery to diseased regions.
A new study addressing this problem has been published in Proceedings of the National Academy of Sciences. The lead author is Khalil Ramadi, a medical engineering and medical physics (MEMP) PhD candidate in the Harvard-MIT Program in Health Sciences and Technology (HST). For this study, Khalil and his thesis advisor, Michael Cima, the David H. Koch Professor of Engineering within the Department of Materials Science and Engineering and the Koch Institute for Integrative Cancer Research, and associate dean of innovation in the School of Engineering, collaborated with Institute Professors Robert Langer and Ann Graybiel to tackle this issue.
The team developed tools to enable targeted delivery of nanoliters of drugs to deep brain structures through chronically implanted microprobes. They also developed nuclear imaging techniques using positron emission tomography (PET) to measure the volume of the brain region targeted with each infusion. “Drugs for disorders of the central nervous system are nonspecific and get distributed throughout the brain,” Cima says. “Our animal studies show that volume is a critical factor when delivering drugs to the brain, as important as the total dose delivered. Using microcannulas and microPET imaging, we can control the area of brain exposed to these drugs, improving targeting accuracy double time comparing to the traditional methods used today.”
The researchers were also able to design cannulas that are MRI-compatible and implanted up to one year in rats. Implanting these cannulas with micropumps allowed the researchers to remotely control the behavior of animals. Significantly, they found that varying the volume infused alone had a profound effect on behavior induced, even if the total drug dose delivered stayed constant. These results show that regulation of volume delivery to brain region is extremely important in influencing brain activity. This technology could potentially enable precise investigation of neurological disease pathology in preclinical models, and more effective treatment in human patients.
Source: Windy Pham – MIT
Publisher: Organized by NeuroscienceNews.com.
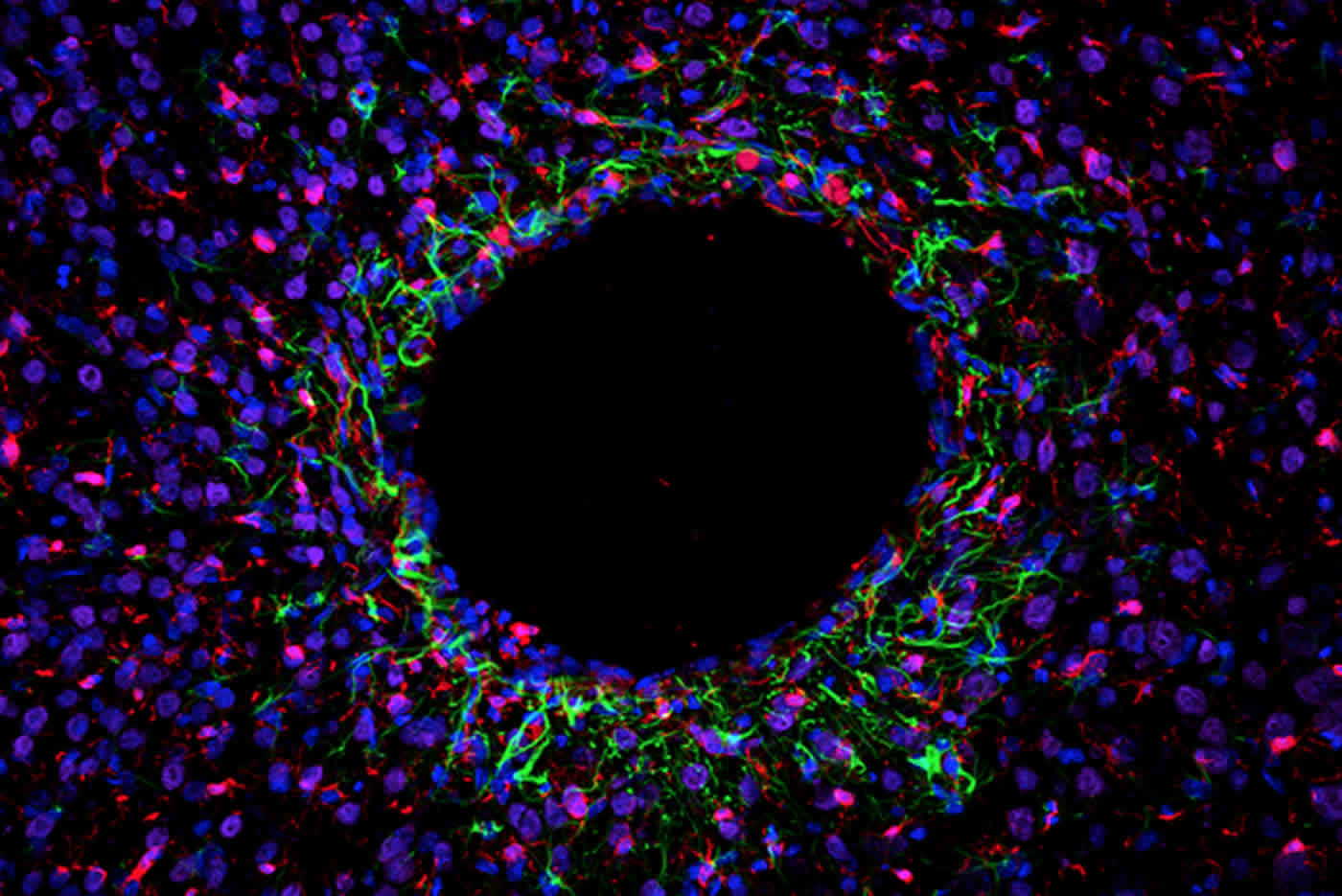
Image Source: NeuroscienceNews.com image is credited to Khalil Ramadi.
Original Research: Abstract for “Focal, remote-controlled, chronic chemical modulation of brain microstructures” by Khalil B. Ramadi, Canan Dagdeviren, Kevin C. Spencer, Pauline Joe, Max Cotler, Erin Rousseau, Carlos Nunez-Lopez, Ann M. Graybiel, Robert Langer, and Michael J. Cima in PNAS. Published June 25 2018.
doi:10.1073/pnas.1804372115
[cbtabs][cbtab title=”MLA”]MIT “Neural Implants Modulate Microstructures in the Brain with Pinpoint Accuracy.” NeuroscienceNews. NeuroscienceNews, 29 June 2018.
<https://neurosciencenews.com/neural-implants-microstructures-9483/>.[/cbtab][cbtab title=”APA”]MIT (2018, June 29). Neural Implants Modulate Microstructures in the Brain with Pinpoint Accuracy. NeuroscienceNews. Retrieved June 29, 2018 from https://neurosciencenews.com/neural-implants-microstructures-9483/[/cbtab][cbtab title=”Chicago”]MIT “Neural Implants Modulate Microstructures in the Brain with Pinpoint Accuracy.” https://neurosciencenews.com/neural-implants-microstructures-9483/ (accessed June 29, 2018).[/cbtab][/cbtabs]
Abstract
Focal, remote-controlled, chronic chemical modulation of brain microstructures
Direct delivery of fluid to brain parenchyma is critical in both research and clinical settings. This is usually accomplished through acutely inserted cannulas. This technique, however, results in backflow and significant dispersion away from the infusion site, offering little spatial or temporal control in delivering fluid. We present an implantable, MRI-compatible, remotely controlled drug delivery system for minimally invasive interfacing with brain microstructures in freely moving animals. We show that infusions through acutely inserted needles target a region more than twofold larger than that of identical infusions through chronically implanted probes due to reflux and backflow. We characterize the dynamics of in vivo infusions using positron emission tomography techniques. Volumes as small as 167 nL of copper-64 and fludeoxyglucose labeled agents are quantified. We further demonstrate the importance of precise drug volume dosing to neural structures to elicit behavioral effects reliably. Selective modulation of the substantia nigra, a critical node in basal ganglia circuitry, via muscimol infusion induces behavioral changes in a volume-dependent manner, even when the total dose remains constant. Chronic device viability is confirmed up to 1-y implantation in rats. This technology could potentially enable precise investigation of neurological disease pathology in preclinical models, and more efficacious treatment in human patients.






