Summary: Mimicking effects of the ketogenic diet with a drug called 2-DG reduced cell excitation and epileptic activity in mouse models of post-traumatic epilepsy. 2-DG may have the potential to restore network function following TBI, reducing the risk of epilepsy associated with head injuries. The findings may have positive implications for people who developed post-traumatic epilepsy, suggesting a change in diet could help alleviate some symptoms.
Source: Tufts University
Neuroscientists led by Chris Dulla at Tufts University School of Medicine prevented the development of epileptic activity in mice after traumatic brain injury by using a drug that mimics the metabolic effects of the ketogenic diet. An advance copy of the study is published today in JCI Insight.
The ketogenic diet was originally developed in the 1920s to treat drug-resistant epilepsy in children. By limiting carbohydrates in the diet, the body is forced to burn fat rather than glucose, the usual source of energy in the body. Although researchers do not know exactly how the therapeutic effects of the diet works, evidence to date suggests the change in metabolism is key.
“While we know the ketogenic diet can control seizures in people with epilepsy, we wanted to learn if it would be able to prevent the development of post-traumatic epilepsy,” says Jenny Koenig, an M.D. and Ph.D. student at Tufts University School of Medicine and the Sackler School of Graduate Biomedical Sciences at Tufts who works in Dulla’s lab.
Post-traumatic epilepsy develops within three years of a traumatic brain injury (TBI) in about 1 out of 10 people. TBIs lead to the dysfunction of the brain’s inhibitory network, including the cells that normally quiet down brain activity. Without inhibition, brain activity increases, causing the behavioral and cognitive challenges seen after injury.
Along with increased activity comes an increased demand for energy production through a process called glycolysis, a system that provides energy to the brain by burning glucose, or sugar. Rather than focus directly on reducing neuronal activity, the research team inhibited glycolysis with a drug called 2-deoxyglucose (2-DG) to mimic the metabolic effects of the ketogenic diet.
By recording brain activity from cells in the injured area with a common electrophysiological technique called whole-cell recording, the researchers determined that excitatory cells were more active in injured tissue, compared to control brain tissue from mice.
Comparatively, the cells which usually inhibit others were dying after injury, leaving the brain without a brake on activity. Application of 2-DG directly on the brain tissue was able to reduce cell excitation and epileptic activity from TBI.
In a follow-up experiment, the research team gave mice 2-DG or saline, as a control, in injection form for one week after injury to assess its effect. They found that 2-DG treatment reduced cell excitation, lessened cell loss, and prevented the development of epileptic brain activity.
“We found that treatment with a small molecule-mimic of the ketogenic diet improves neuronal survival and brain function after TBI. We also established that different types of neurons use energy in different ways, allowing cell type-specific manipulation of neuronal metabolism,” said Dulla, whose lab at Tufts University School of Medicine explores the function of neuronal networks, particularly as they relate to epilepsy and other neurological diseases.
“While preliminary, our study suggests that manipulating brain metabolism – through a specific diet or a mimic of that – could be an effective way to prevent the very development of epilepsy or epileptogenesis after TBI and restore normal synaptic communication in the brain,” he continued. “Importantly, 2-DG is already being investigated to help treat cancer and other diseases, suggesting this approach might be used clinically if properly tested in brain injury.”
The authors caution that long-term exposure to 2-DG has been associated with cardiac toxicity.
Additionally, the research group did not investigate the specific cells impacted by 2-DG but note that the results point to a new therapeutic path for post-traumatic epilepsy prevention.
Additional authors are David Cantu (co-corresponding author), formerly of Tufts University School of Medicine (TUSM); Cho Low, a graduate of the Sackler School; Mary Sommer, TUSM; Farzad Noubary, Northeastern University; Danielle Croker, formerly of Tufts; Michael Whalen, Harvard Medical School; and Dong Kong, TUSM.
Funding: This work was supported by National Institutes of Health’s National Institute of Neurological Disorders and Stroke (R21NS098009 and F31NS101741, a Ruth L. Kirschstein Predoctoral Individual National Research Service Award) and the United States Department of Defense (W81XWH-16-ERP-IDA). The authors have no conflicts of interest to disclose. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders.
Source:
Tufts University
Media Contacts:
Siobhan Gallagher – Tufts University
Image Source:
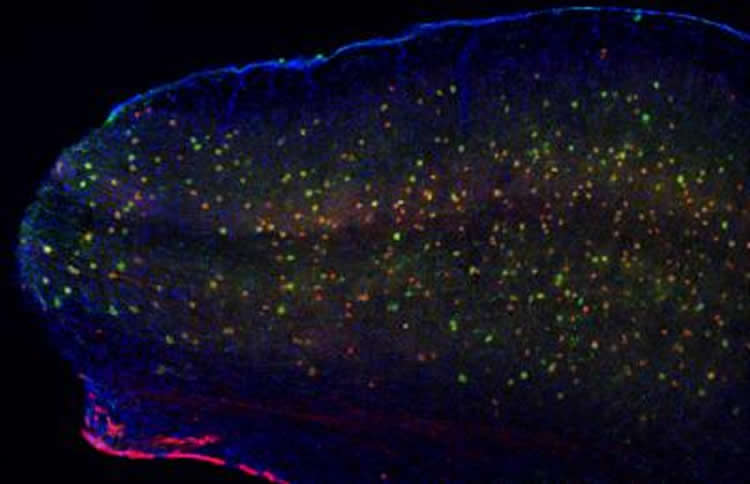
The image is credited to Chris Dulla laboratory/Tufts University School of Medicine.
Original Research: Closed access
“Brain Amygdala Volume Increases in Veterans and Active-Duty Military Personnel With Combat-Related Posttraumatic Stress Disorder and Mild Traumatic Brain Injury”. Koenig, J., Cantu, D., Low, C., Sommer, M., Noubary, F., Croker, D., Whalen, M., Kong, D., Dulla, C. JCI Insight. doi:10.1172/jci.insight.126506
Abstract
Brain Amygdala Volume Increases in Veterans and Active-Duty Military Personnel With Combat-Related Posttraumatic Stress Disorder and Mild Traumatic Brain Injury
Traumatic brain injury (TBI) causes cortical dysfunction and can lead to post-traumatic epilepsy. Multiple studies demonstrate that GABAergic inhibitory network function is compromised following TBI, which may contribute to hyperexcitability and motor, behavioral, and cognitive deficits. Preserving the function of GABAergic interneurons, therefore, is a rational therapeutic strategy to preserve cortical function after TBI and prevent long-term clinical complications. Here, we explored an approach based on the ketogenic diet, a neuroprotective and anticonvulsant dietary therapy which results in reduced glycolysis and increased ketosis. Utilizing a pharmacologic inhibitor of glycolysis (2-deoxyglucose, or 2-DG), we found that acute in vitro application of 2-DG decreased the excitability of excitatory neurons, but not inhibitory interneurons, in cortical slices from naïve mice. Employing the controlled cortical impact (CCI) model of TBI in mice, we found that in vitro 2-DG treatment rapidly attenuated epileptiform activity seen in acute cortical slices 3 to 5 weeks after TBI. One week of in vivo 2-DG treatment immediately after TBI prevented the development of epileptiform activity, restored excitatory and inhibitory synaptic activity, and attenuated the loss of parvalbumin-expressing inhibitory interneurons. In summary, 2-DG may have therapeutic potential to restore network function following TBI.






