Summary: Researchers uncovered a key mechanism of aging – improper calcium signaling in the mitochondria of certain immune cells, leading to chronic inflammation.
As we age, these mitochondria in macrophages lose their ability to uptake and utilize calcium, contributing to various age-related conditions. However, by increasing calcium uptake in these cells, the researchers believe we could potentially prevent harmful inflammation and slow down aging.
Key Facts:
- Mitochondria in immune cells, known as macrophages, lose their ability to process calcium as they age, leading to chronic inflammation and accelerating aging.
- The researchers believe increasing calcium uptake in these mitochondrial macrophages could prevent harmful inflammation, thereby slowing the aging process.
- This discovery opens up new therapeutic strategies for age-associated inflammation, and could potentially impact cardiometabolic and neurodegenerative diseases.
Source: University of Virginia
University of Virginia School of Medicine researchers have discovered a key driver of chronic inflammation that accelerates aging.
That finding could let us slow the clock to live longer, healthier lives, and may allow us to prevent age-related conditions such as deadly heart disease and devastating brain disorders that rob us of our faculties.

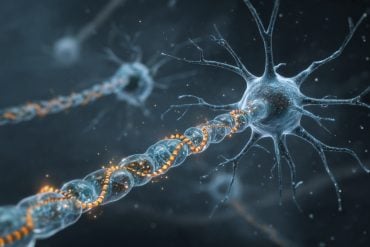
So what drives this harmful inflammation? The answer is improper calcium signaling in the mitochondria of certain immune cells. Mitochondria are the power generators in all cells, and they rely heavily on calcium signaling.
The UVA Health researchers, led by Bimal N. Desai, PhD, found that mitochondria in immune cells called macrophages lose their ability to take up and use calcium with age. This, the researchers show, leads to chronic inflammation responsible for many of the ailments that afflict our later years.
The researchers believe that increasing calcium uptake by the mitochondrial macrophages could prevent the harmful inflammation and its terrible effects. Because macrophages reside in all organs of our bodies, including the brain, targeting such “tissue-resident macrophages” with appropriate drugs may allow us to slow age-associated neurodegenerative diseases.
“I think we have made a key conceptual breakthrough in understanding the molecular underpinnings of age-associated inflammation,” said Desai, of UVA’s Department of Pharmacology and UVA’s Carter Immunology Center.
“This discovery illuminates new therapeutic strategies to interdict the inflammatory cascades that lie at the heart of many cardiometabolic and neurodegenerative diseases.”
The Inflammation of Aging – ‘Inflammaging’
Macrophages are white blood cells that play critical roles in our immune systems and, in turn, our good health. They swallow up dead or dying cells, allowing our bodies to remove cellular debris, and patrol for pathogens and other foreign invaders. In this latter role, they act as important sentries for our immune systems, calling for help from other immune cells as needed.
Scientists have known that macrophages become less effective with age, but it has been unclear why. Desai’s new discovery suggests answers.
Desai and his team say their research has identified a “keystone” mechanism responsible for age-related changes in the macrophages.
These changes, the scientists believe, make the macrophages prone to chronic, low-grade inflammation at the best of times. And when the immune cells are confronted by an invader or tissue damage, they can become hyperactive. This drives what is known as “inflammaging” – chronic inflammation that drives aging.
Further, the UVA Health scientists suspect that the mechanism they have discovered will hold true not just for macrophages but for many other related immune cells generated in the bone marrow.
That means we may be able to stimulate the proper functioning of those cells as well, potentially giving our immune systems a big boost in old age, when we become more susceptible to disease.
Next Steps
Fixing “inflammaging” won’t be as simple as taking a calcium supplement. The problem isn’t a shortage of calcium so much as the macrophages’ inability to use it properly.
But Desai’s new discovery has pinpointed the precise molecular machinery involved in this process, so we should be able to discover ways to stimulate this machinery in aging cells.
“This highly interdisciplinary research effort, at the interface of computational biology, immunology, cell biology and biophysics, wouldn’t have been possible without the determination of Phil Seegren, the graduate student who spearheaded this ambitious project,” Desai said.
“Now, moving forward, we need an equally ambitious effort to figure out the wiring that controls this mitochondrial process in different types of macrophages and then manipulate that wiring in creative ways for biomedical impact.”
Aging Findings Published
The researchers have published their findings in the scientific journal Nature Aging. The article is open access, meaning it is free to read.
The research team consisted of Seegren, Logan R. Harper, Taylor K. Downs, Xiao-Yu Zhao, Shivapriya B. Viswanathan, Marta E. Stremska, Rachel J. Olson, Joel Kennedy, Sarah E. Ewald, Pankaj Kumar and Desai. The scientists reported that they have no financial interests in the work.
Funding: The research was supported by the National Institutes of Health, grants AI155808, GM108989, GM138381, P30 CA044579 and T32 GM007055-46, and by the Owens Family Foundation.
About this aging and inflammation research news
Author: Josh Barney
Source: University of Virginia
Contact: Josh Barney – University of Virginia
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Reduced mitochondrial calcium uptake in macrophages is a major driver of inflammaging” by Bimal N. Desai et al. Nature Aging
Abstract
Reduced mitochondrial calcium uptake in macrophages is a major driver of inflammaging
Mitochondrial dysfunction is linked to age-associated inflammation or inflammaging, but underlying mechanisms are not understood. Analyses of 700 human blood transcriptomes revealed clear signs of age-associated low-grade inflammation.
Among changes in mitochondrial components, we found that the expression of mitochondrial calcium uniporter (MCU) and its regulatory subunit MICU1, genes central to mitochondrial Ca2+ (mCa2+) signaling, correlated inversely with age. Indeed, mCa2+ uptake capacity of mouse macrophages decreased significantly with age.
We show that in both human and mouse macrophages, reduced mCa2+ uptake amplifies cytosolic Ca2+ oscillations and potentiates downstream nuclear factor kappa B activation, which is central to inflammation.
Our findings pinpoint the mitochondrial calcium uniporter complex as a keystone molecular apparatus that links age-related changes in mitochondrial physiology to systemic macrophage-mediated age-associated inflammation.
The findings raise the exciting possibility that restoring mCa2+ uptake capacity in tissue-resident macrophages may decrease inflammaging of specific organs and alleviate age-associated conditions such as neurodegenerative and cardiometabolic diseases.