Summary: A rare genetic mutation known as APOE3-R136S, or the “Christchurch mutation,” appears to protect against Alzheimer’s disease by suppressing inflammatory signaling in the brain’s immune cells. Researchers found that this mutation dampens the cGAS-STING pathway, a key innate immune mechanism that is abnormally activated in Alzheimer’s and other neurodegenerative disorders.
Mice engineered with the mutation showed less tau accumulation, synaptic damage, and brain dysfunction—hallmarks of Alzheimer’s—despite having high amyloid levels. The findings suggest that targeting cGAS-STING could mimic the mutation’s protective effects and offer a new route for treating Alzheimer’s.
Key Facts:
- Protective Pathway Identified: The Christchurch mutation suppresses cGAS-STING, a key immune pathway in Alzheimer’s.
- Drug Potential: Blocking this pathway in mice mirrored the mutation’s protective effects on brain function.
- Focus Shift: Findings support the idea that inflammation and tau—not just amyloid—drive Alzheimer’s progression.
Source: Weill Cornell University
A rare gene mutation that delays Alzheimer’s disease does so by damping inflammatory signaling in brain-resident immune cells, according to a preclinical study led by investigators at Weill Cornell Medicine.
The finding adds to growing evidence that brain inflammation is a major driver of neurodegenerative disorders such as Alzheimer’s—and that it may be a key therapeutic target for these disorders.

In the study, published June 23 in Immunity, the researchers examined the effects of the mutation APOE3-R136S—known as the “Christchurch mutation”—which was recently found to delay hereditary early-onset Alzheimer’s.
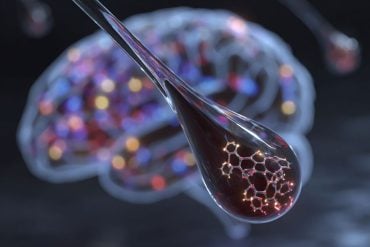
The Weill Cornell Medicine scientists showed that the mutation inhibits the cGAS-STING pathway, an innate immune signaling cascade that is abnormally activated in Alzheimer’s and other neurodegenerative diseases.
The researchers found that pharmacologically blocking the cGAS-STING pathway with a drug-like inhibitor replicated key protective effects of the mutation in a preclinical model.
“This is an exciting study because it suggests that inhibiting this cGAS-STING pathway could make the brain more resistant to the Alzheimer’s process, even in the face of significant tau accumulation,” said study senior author Dr. Li Gan, the Burton P. and Judith B. Resnick Distinguished Professor in Neurodegenerative Diseases and director of the Helen and Robert Appel Alzheimer’s Disease Research Institute at Weill Cornell Medicine.
The study’s co-first authors were Drs. Sarah Naguib, Chloe Lopez-Lee and Eileen Ruth Torres, all postdoctoral researchers in the Gan Laboratory during the study.
Alzheimer’s disease, which afflicts at least seven million adults in the United States, has long defied scientific efforts to understand its causes and develop effective treatments. Growing evidence suggests that tau—not amyloid—is the key driver of neurodegeneration and cognitive decline.
What determines an individual’s susceptibility or resistance to tau toxicity remains poorly understood. The Christchurch mutation, which protects against tau pathology and cognitive deterioration despite extensive amyloid buildup, offers an important clue.
This rare mutation is found in the APOE gene encoding a cholesterol transport protein (apolipoprotein E), and was first discovered by a laboratory in Christchurch, New Zealand. In 2019, scientists studying a Colombian family with hereditary early-onset Alzheimer’s, which typically strikes by age 50, reported that one family member, who had two copies of the Christchurch mutation, remained cognitively healthy into her 70s.
Despite high brain amyloid, she exhibited low levels of tau. Subsequent research, mostly in mouse models, has confirmed the Christchurch mutation’s beneficial effects—but researchers still aren’t sure how it exerts protection.
In the new study, Dr. Gan’s team engineered the Christchurch mutation into the APOE gene in mice that develop tau accumulation, and found that it protected the animals from hallmark Alzheimer’s features—including tau accumulation, synaptic damage, and disruptions in brain
activity. These protective effects were traced to suppression of the cGAS-STING pathway, an innate immune signaling cascade normally activated in response to viral threat but is chronically activated in Alzheimer’s disease.
“We are particularly encouraged that this mutation ameliorates disease at the level of brain function, which has not been shown before,” Dr. Naguib said.
Dr. Gan and colleagues further discovered that the protective mechanism of the Christchurch mutation can be largely attributed to taming microglia, brain-resident immune cells. These cells and their inflammatory state in Alzheimer’s have long been seen as potential drivers of the disease process.
When the researchers treated mice with tau pathology using a small-molecule inhibitor of cGAS-STING signaling, they observed synapse-protecting effects and molecular changes in brain cells that closely resembled those seen with the protective mutation.
With mounting evidence that cGAS-STING signaling contributes to disease progression, the team is now exploring its role in other neurodegenerative disorders and testing inhibitors on different animal models of these disorders.
“We can’t engineer the rare Christchurch mutation into people to prevent Alzheimer’s,” Dr. Gan said, “But targeting the same pathway it modulates—cGAS-STING—could offer a new therapeutic strategy for Alzheimer’s, and potentially other neurodegenerative conditions.”
About this genetics and Alzheimer’s disease research news
Author: Barbara Prempeh
Source: Weill Cornell University
Contact: Barbara Prempeh – Weill Cornell University
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“The R136S mutation in the APOE3 gene confers resilience against tau pathology via inhibition of the cGAS-STING-IFN pathway” by Li Gan et al. Immunity
Abstract
The R136S mutation in the APOE3 gene confers resilience against tau pathology via inhibition of the cGAS-STING-IFN pathway
The Christchurch mutation (R136S) in the APOE3 (E3S/S) gene is associated with attenuated tau load and cognitive decline despite the presence of a causal PSEN1 mutation and high amyloid burden in the carrier.
However, the molecular mechanisms enabling the E3S/S mutation to mitigate tau-induced neurodegeneration remain unclear.
Here, we replaced mouse Apoe with wild-type human APOE3 or APOE3S/S on a tauopathy background.
The R136S mutation decreased tau load and protected against tau-induced synaptic loss, myelin loss, and reduction in hippocampal theta and gamma power.
Additionally, the R136S mutation reduced interferon responses to tau pathology in both mouse and human microglia, suppressing cGAS-STING pathway activation.
Treating E3 tauopathy mice with a cGAS inhibitor protected against tau-induced synaptic loss and induced transcriptomic alterations similar to the R136S mutation across brain cell types.
Thus, suppression of the microglial cGAS-STING-interferon (IFN) pathway plays a central role in mediating the protective effects of R136S against tauopathy.