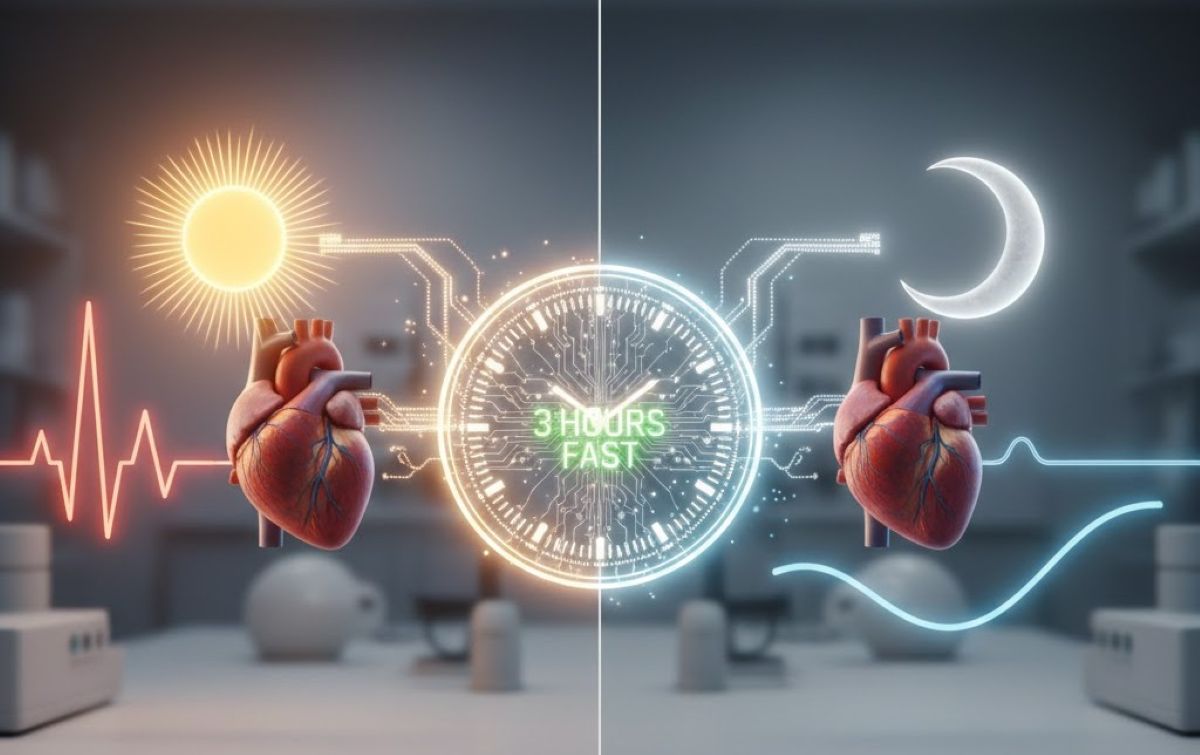
Summary: A new study has demonstrated that the timing of food intake relative to sleep is just as critical as the duration of the fast itself. By aligning overnight fasting with an individual’s circadian rhythm—specifically by finishing meals at least three hours before bedtime—researchers saw significant improvements in cardiovascular and metabolic markers without reducing total caloric intake.
This “sleep-anchored” approach improved blood pressure dipping and heart rate variability, suggesting that working with the body’s natural clock can strengthen the coordination between the heart, metabolism, and sleep to protect against chronic disease.
Key Facts
- Circadian Alignment: The study emphasized finishing all food intake three hours before bedtime and dimming lights during that period to align with the body’s natural sleep-wake cycle.
- Cardiovascular “Dipping”: Participants in the intervention group saw a 3.5% drop in nighttime blood pressure and a 5% drop in heart rate, creating a healthier day-night physiological pattern.
- Metabolic Efficiency: Daytime blood-sugar control improved as the pancreas responded more efficiently to glucose challenges, despite no change in what or how much participants ate.
- High Adherence: The study reported a 90% adherence rate, suggesting that using sleep as an “anchor” for fasting is a more sustainable lifestyle change than traditional calorie restriction for many adults.
Source: Northwestern University
A new Northwestern Medicine study has personalized overnight fasting by aligning it with individuals’ circadian sleep-wake rhythm — an important regulator of cardiovascular and metabolic function — without changing their caloric intake.
The study found that among middle-age and older adults who are at higher risk for cardiometabolic disease, extending the participants’ overnight fast by about two hours, dimming the lights and not eating for three hours prior to bedtime improved measures of cardiovascular and metabolic health during sleep, as well as during the daytime.
“Timing our fasting window to work with the body’s natural wake-sleep rhythms can improve the coordination between the heart, metabolism and sleep, all of which work together to protect cardiovascular health,” said first author Dr. Daniela Grimaldi, research associate professor of neurology in the division of sleep medicine at Northwestern University Feinberg School of Medicine.
The study will be published Feb. 12 in the journal Arteriosclerosis, Thrombosis, and Vascular Biology, part of the American Heart Association.
“It’s not only how much and what you eat, but also when you eat relative to sleep that is important for the physiological benefits of time-restricted eating,” said corresponding author Dr. Phyllis Zee, director of the Center for Circadian and Sleep Medicine and the chief of sleep medicine in the department of neurology at Feinberg.
Previous research has found only 6.8% of U.S. adults had optimal cardiometabolic health in 2017 to 2018. Poor cardiometabolic health can lead to chronic illness, including type 2 diabetes, non-alcoholic fatty liver disease and cardiovascular diseases.
Time-restricted eating has continued to surge in popularity because research has shown it can improve cardiometabolic health and rival traditional calorie‑restricted diets, but most studies have focused on how long people fast, not how their fast lines up with their sleep schedule — a key factor in metabolic regulation.
Given the nearly 90% adherence rate in the study, the study’s novel approach of leveraging the sleep period as an anchor for the timing of time-restricted eating may be a more accessible non-pharmacological strategy for improving cardiometabolic health, particularly in middle-aged and older adults who are at higher risk for cardiometabolic disease, the study authors said.
The study authors said they plan refine the protocol from this study and take it to larger multi-center trials.
Improved blood pressure, heart rate, blood-sugar control
In the 7.5‑week study, people who finished eating at least three hours before going to bed saw meaningful improvements compared with those who kept their usual eating routines. They experienced:
- Improved nighttime patterns in blood pressure (dipping by 3.5%) and heart rate (dipping by 5%): Their bodies showed a more natural drop in both measures during sleep, which is an important sign of cardiovascular health. Notably, their hearts beat faster during the day when they were active and slowed at night when they were resting. A stronger day-night pattern is linked to better cardiovascular health.
- Better daytime blood‑sugar control: Their pancreas responded more efficiently when challenged with glucose, suggesting it could release insulin more effectively and keep blood sugar steadier.
In the study, 39 overweight/obese participants (36 to 75 years old) completed either an extended overnight fasting intervention (13 to 16 hours of fasting) or a control condition (habitual fast of 11 to 13 hours). Both groups dimmed the lights three hours before bedtime. The intervention group consisted of 80% women.
Key Questions Answered:
A: Yes, it matters. This study suggests that even if you fast for a long period, eating close to bedtime disrupts the natural nighttime “dip” in blood pressure and heart rate. Aligning the fast so you stop eating three hours before sleep is what triggered the cardiovascular benefits.
A: Absolutely. The participants in this study didn’t change what they ate or how much they ate—only when they ate. The health improvements came entirely from the timing shift, not from weight loss or calorie counting.
A: Dimming the lights helps signal the body to begin its natural transition into sleep mode. This supports the circadian rhythm, which in turn helps regulate how the heart and metabolism function during the overnight fast.
Editorial Notes:
- This article was edited by a Neuroscience News editor.
- Journal paper reviewed in full.
- Additional context added by our staff.
About this circadian rhythm and cardiovascular health research news
Author: Kristin Samuelson
Source: Northwestern University
Contact: Kristin Samuelson – Northwestern University
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Sleep-aligned Extended Overnight Fasting Improves Nighttime and Daytime Cardiometabolic Function” by Daniela Grimaldi, Kathryn J. Reid, Sabra M. Abbott, Kristen L. Knutson, and Phyllis C. Zee. Arteriosclerosis Thrombosis and Vascular Biology
DOI:10.1161/ATVBAHA.125.323355
Abstract
Sleep-aligned Extended Overnight Fasting Improves Nighttime and Daytime Cardiometabolic Function
BACKGROUND:
Time-restricted eating has gained attention for its potential cardiometabolic health benefits. Existing time-restricted eating approaches may have limited adherence and sustainability due to fixed fasting windows with prolonged fasting duration before sleep, or they involve self-selected fasting windows without specifying the duration relative to sleep, a critical period for cardiometabolic regulation.
We hypothesized that an individualized approach that extended overnight fasting duration by 3 hours in alignment with habitual sleep time (last meal ≥3 hours before sleep) would enhance nighttime autonomic balance, decrease blood pressure and heart rate, increase blood pressure per hour dipping, and glucose regulation compared with a control group maintaining habitual eating patterns.
METHODS:
In this randomized parallel-arm controlled trial, 39 overweight/obese participants (36–75 years) completed either an extended overnight fasting intervention (13–16-hour fasting) or a control condition (habitual fast of 11–13 hours). Both groups dimmed lights 3 hours before bedtime. The intervention duration was 7.5 weeks.
RESULTS:
Compared with control, extended overnight fasting intervention significantly improved the coprimary outcome of nighttime dipping of diastolic blood pressure, but not the Matsuda Index of insulin sensitivity. extended overnight fasting improved secondary measures of nighttime autonomic function and morning oral glucose tolerance, including lower nighttime heart rate, higher heart rate variability, lower nighttime cortisol, and during the Oral Glucose Tolerance Test, lower glucose level, and higher 30-minute insulinogenic index, indicating improved acute insulin response.
CONCLUSIONS:
Extending overnight fasting duration by 3 hours in alignment with sleep improved cardiometabolic health in middle-aged/older adults by strengthening coordination between circadian- and sleep-regulated autonomic and metabolic activity. This sleep-aligned time-restricted eating approach represents a novel, accessible lifestyle intervention with promising potential for improving cardiometabolic function.