Summary: A new study reports that increased volume in the choroid plexus appears to be associated with greater cognitive impairment and Alzheimer’s disease.
Source: RSNA
Increased volume of an important structure in the brain called the choroid plexus is linked to greater cognitive impairment and Alzheimer’s disease, according to a new study published in the journal Radiology.
The choroid plexus is a network of blood vessels, connective tissue and cells found in spaces of the brain called ventricles. The plexus plays an important role in brain health. It is a gateway for immune cells from the blood to the brain. As the primary site for the production of cerebrospinal fluid, it is crucial to clearing waste products and toxic proteins from brain cells.
This role is particularly important in the case of Alzheimer’s disease. Recent research suggests that disease progression is related to the accumulation of abnormal proteins called amyloid and tau and subsequent degeneration of the nerves.
“Researchers believe impaired clearance rather than overproduction of abnormal amyloid and tau is responsible for Alzheimer’s disease,” said study senior author Won-Jin Moon, M.D., Ph.D., professor of radiology and chairperson of the Department of Radiology at the Konkuk University School of Medicine in Seoul, Korea.
“Thus, we assume that the abnormal status of choroid plexus is linked to the failure of clearance leading to waste and toxic protein accumulation in the brain and failure of immune surveillance leading to neuroinflammation.”
Little is known about the choroid plexus’ imaging profile in cognitive impairment.
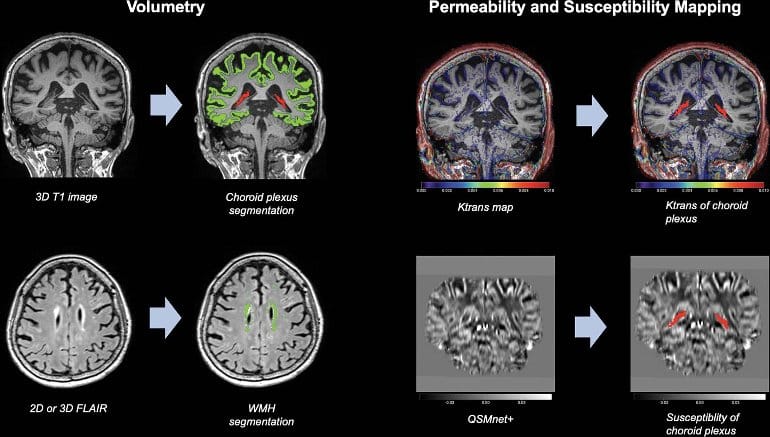
To learn more, Dr. Moon and colleagues performed brain MRI on 532 participants at various stages of cognitive impairment. Of the 532 participants, 132 underwent permeability imaging using dynamic contrast-enhanced MRI.
Choroid plexus volume and permeability were associated with the severity of cognitive impairment on brain MRI. Choroid plexus volume was greater in those with Alzheimer’s dementia than in those without. Higher choroid plexus volume was negatively associated with memory. It also had negative effects on executive function, a wide-ranging set of mental skills governing things like self-control and planning.
“Our study found that the enlarged choroid plexus volume is independently associated with increased cognitive impairment,” Dr. Moon said.
“We found no relationship between choroid plexus volume and amyloid pathology but a clear relationship between the choroid plexus volume and cognitive impairment severity.”
The study results point to new possibilities for MRI’s role in the diagnosis of Alzheimer’s disease.
“I think our findings on the choroid plexus can suggest it as a new potential MR imaging surrogate for an impaired clearance system and neuroinflammation,” Dr. Moon said.
Other potential clinical applications include helping researchers develop new target drugs or treatments for clearance failure and neuroinflammation. Eventually, choroid plexus measurements could help speed treatment to those who need it most.
“If we combine choroid plexus volume and hippocampal volume in a screening stage, it may help us better discriminate the more vulnerable patients from the less vulnerable ones,” Dr. Moon said.
The researchers plan to follow up with a longitudinal study. They will explore changes in choroid plexus volume over time as the disease progresses.
About this Alzheimer’s disease research news
Author: Linda Brooks
Source: RSNA
Contact: Linda Brooks – RSNA
Image: The image is credited to RSNA
Original Research: Open access.
“Choroid Plexus Volume and Permeability at Brain MRI within the Alzheimer Disease Clinical Spectrum” by Jong Duck Choi et al. Radiology
Abstract
Choroid Plexus Volume and Permeability at Brain MRI within the Alzheimer Disease Clinical Spectrum
Background
Mounting evidence suggests that the choroid plexus (CP) plays an important role in the pathophysiology of Alzheimer disease (AD), but its imaging profile in cognitive impairment remains unclear.
Purpose
To evaluate CP volume, permeability, and susceptibility by using MRI in patients at various stages of cognitive impairment.
Materials and Methods
This retrospective study evaluated patients with cognitive symptoms who underwent 3.0-T MRI of the brain, including dynamic contrast-enhanced (DCE) imaging and quantitative susceptibility mapping (QSM), between January 2013 and May 2020. CP volume was automatically segmented using three-dimensional T1-weighted sequences; the volume transfer constant (ie, Ktrans) and fractional plasma volume (ie, Vp) were determined using DCE MRI, and susceptibility was assessed using QSM. The effects of CP volume, expressed as the ratio to intracranial volume, on cognition were evaluated using multivariable linear regression adjusted for age, sex, education, apolipoprotein E ε4 allele status, and volumetric measures.
Results
A total of 532 patients with cognitive symptoms (mean age, 72 years ± 9 [SD]; 388 women) were included: 78 with subjective cognitive impairment (SCI), 158 with early mild cognitive impairment (MCI), 149 with late MCI, and 147 with AD. Among these, 132 patients underwent DCE MRI and QSM. CP volume was greater in patients at more severe stages (ratio of intracranial volume × 103: 0.9 ± 0.3 for SCI, 1.0 ± 0.3 for early MCI, 1.1 ± 0.3 for late MCI, and 1.3 ± 0.4 for AD; P < .001). Lower Ktrans (r = –0.19; P = .03) and Vp (r = –0.20; P = .02) were negatively associated with CP volume; susceptibility was not (r = 0.15; P = .10). CP volume was negatively associated with memory (B = –0.67; standard error of the mean [SEM], 0.21; P = .01), executive function (B = –0.90; SEM, 0.31; P = .01), and global cognition (B = –0.82; SEM, 0.32; P = .01).
Conclusion
Among patients with cognitive symptoms, larger choroid plexus volume was associated with severity of cognitive impairment in the Alzheimer disease spectrum.