About half of all patients with Alzheimer’s disease develop symptoms of psychosis, such as delusions or hallucinations.
But the pathological mechanisms that underlie psychotic symptoms are unclear, limiting the ability to manage and treat them. Some studies have suggested they are related to the underlying causes of Alzheimer’s disease such as the protein deposits found in the brains of Alzheimer’s patients, but others found no correlation.
A study published today in the Journal of Alzheimer’s Disease found that cerebrovascular disease is a major determinant of psychosis in people with Alzheimer’s disease. Cerebrovascular disease is a group of conditions that restrict the circulation of blood to the brain.
Using data from the National Alzheimer’s Coordinating Centre database collected from 29 Alzheimer’s disease centres in the United States between 2005 and 2012, researchers led by Dr. Corinne Fischer, a psychiatrist and researcher at St. Michael’s Hospital, analyzed autopsy data from 1,073 people.
Of the 890 people who had been clinically diagnosed with Alzheimer’s while they were alive, the people most likely to be psychotic were those whose autopsies showed they had more physical signs of Alzheimer’s such as neuritic plaques (protein deposits) and neurofibrillary tangles (twisted fibers found inside brain cells).
But when they looked at the 728 people whose autopsies confirmed they had Alzheimer’s, those with psychosis did not show increased physical evidence of Alzheimer’s disease. Alzheimer’s can only be confirmed through an autopsy, so some patients in the clinically diagnosed group had been misdiagnosed with Alzheimer’s.
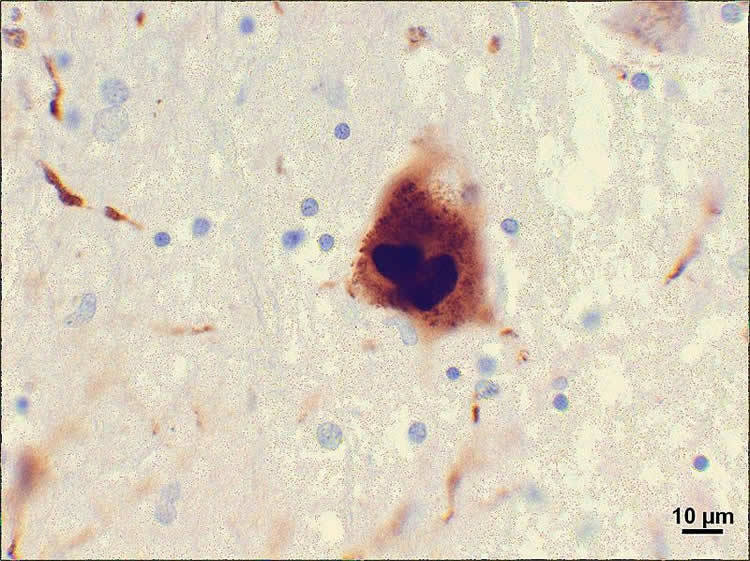
In both groups of patients, psychosis correlated significantly with Lewy bodies, abnormal protein aggregates found in nerve cells of patients with Parkinson’s disease. This was not an unexpected finding since psychosis is prominent when dementia accompanies Parkinson’s disease.
What was entirely unexpected was the prominent role in psychosis of vascular risk factors (hypertension, diabetes, age at quitting smoking) and cerebral injuries related to small vessel disease,
About 19 per cent of people with Alzheimer’s who live in the community (rather than in institutions) are thought to have delusions and 14 per cent have hallucinations. Psychotic symptoms are significant in Alzheimer’s patients because they have been shown to be associated with increased burden on caregivers, increased functional decline and more rapid progression of the disease.
Funding: This study received funding from the Canadian Institutes of Health Research.
Source: Kendra Stephenson – St. Michael’s Hospital
Image Credit: The image is credited to Suraj Rajan and is licensed CC BY SA 3.0
Original Research: Abstract for “Lewy Bodies, Vascular Risk Factors, and Subcortical Arteriosclerotic Leukoencephalopathy, but not Alzheimer Pathology, are Associated with Development of Psychosis in Alzheimer’s Disease” by Fischer, Corinne E.; Qian, Winnie; Schweizer, Tom A.; Millikin, Colleen P.; Ismail, Zahinoor; Smith, Eric E.; Lix, Lisa M.; Shelton, Paul; and Munoz, David G. in Journal of Alzheimer’s Disease. Published online December 21 2015 doi:10.3233/JAD-150606
Abstract
Lewy Bodies, Vascular Risk Factors, and Subcortical Arteriosclerotic Leukoencephalopathy, but not Alzheimer Pathology, are Associated with Development of Psychosis in Alzheimer’s Disease
Background: The neuropathological correlates of psychosis in Alzheimer’s disease (AD) is unclear, with some studies reporting a correlation between psychosis and increased AD pathology while others have found no association. Objective:To determine the demographic, clinical, and neuropathological features associated with psychotic symptoms in clinically attributed and neuropathologically proven AD.
Method: We separately reviewed two overlapping groups of clinically diagnosed (cAD) AD patients with neuropathology data and neuropathologically definite (npAD) cases (regardless of clinical diagnosis) from the NACC database, and explored the relationships between psychosis and clinical variables, neuropathologic correlates, and vascular risk factors. Delusions and hallucinations, defined according to the NPI-Q, were analyzed separately. Results:1,073 subjects in the database fulfilled our criteria (890 cAD and 728 npAD patients). 34% of cAD and 37% of npAD had psychotic symptoms during their illness. Hallucinations were associated with greater cognitive and functional impairments on the MMSE and CDR, while delusional patients showed less impairment on CDR, consistent across cAD and npAD groups. Burden of AD pathology appears to relate to presence of psychotic symptoms in the clinical AD group, but this result is not confirmed in the neuropathologically confirmed group suggesting the findings in the clinical group were due to misdiagnosis of AD. Lewy body pathology, subcortical arteriosclerotic leukoencephalopathy, and vascular risk factors, including a history of hypertension and diabetes, were associated with the development of psychosis.
Method: Vascular and Lewy body pathologies and vascular risk factors are important modifiers of the risk of psychosis in AD.
“Lewy Bodies, Vascular Risk Factors, and Subcortical Arteriosclerotic Leukoencephalopathy, but not Alzheimer Pathology, are Associated with Development of Psychosis in Alzheimer’s Disease” by Fischer, Corinne E.; Qian, Winnie; Schweizer, Tom A.; Millikin, Colleen P.; Ismail, Zahinoor; Smith, Eric E.; Lix, Lisa M.; Shelton, Paul; and Munoz, David G. in Journal of Alzheimer’s Disease. Published online December 21 2015 doi:10.3233/JAD-150606







