Summary: Teenagers who were exposed to alcohol while in the womb are more likely to have disruptions in neural connections through the corpus callosum, which can lead to cognitive impairment and a range of neurological, and psychological disorders. Researchers recommend pregnant women completely abstain from drinking alcohol.
Source: AIP
An international group of researchers has taken one of the first major steps in finding the biological changes in the brain that drive fetal alcohol spectrum disorder (FASD). New work using chaos theory to analyze brain signals, discussed this month in the journal Chaos, from AIP Publishing, shows the long-term effects.
Researchers found that teenagers who were exposed to alcohol while in the womb showed altered brain connections that were consistent with impaired cognitive performance. Their findings were reached by measuring the responses from a brain imaging technique called magnetoencephalography (MEG) and then analyzing them with tools developed using chaos theory.
FASD is one of the leading causes of intellectual disability worldwide and is linked to a wide array of neurological issues, including ADHD. While the prevailing theory links expectant mothers’ alcohol consumption to cognitive impairments for children, questions about the extent of this effect remain. Despite the known link, researchers are uncertain about the precise mechanism by which alcohol alters the developing brain.
The group’s efforts mark one of the first times researchers have been able to quantify the effects of alcohol exposure on the developing brain.
“The paper provides important integrative results for the field of FASD,” said Julia Stephen, an author on the paper.
“These results may then indicate that simple sensory measures may provide sensitivity for brain deficits that affect the broader cognitive domain.”
Previous attempts to study the brain circuitry in affected individuals have been hampered by the difficulty of drawing conclusions from complicated MEG data.
To get to the heart of the problem, members of the team developed a sophisticated computer technique called Cortical Start Spatio-Temporal multidipole analysis that could identify which areas of the brain were active when research subjects were in the MEG machine.
After data from 19 FASD patients and 21 subjects without FASD was collected, the computational approach revealed several areas of the brain that showed impaired connectivity among the FASD group.
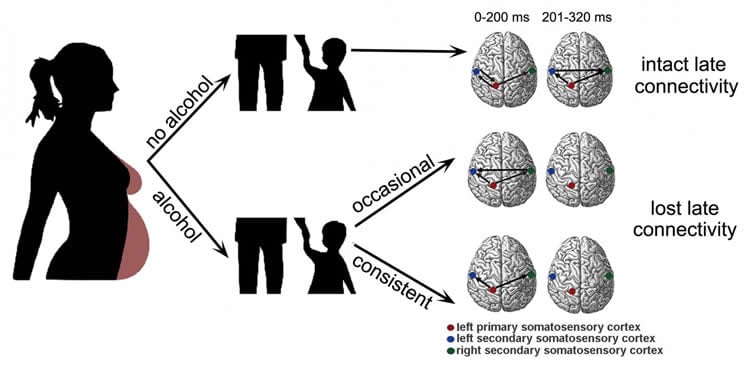
Subjects who were exposed to alcohol in the womb were more likely to have issues with connections through their corpus callosum, the band of brain tissue that connects the left and right halves of the brain. Deficits in this area have been reported in people with schizophrenia, multiple sclerosis, autism, depression and abnormalities in sensation.
“This work presents major evidence that children exposed to alcohol prenatally are at risk of suffering from impaired cognitive abilities and other secondary factors,” said Lin Gao, an author on the paper. “Our study … shows that there is no safe amount or safe stages during pregnancy for alcohol consumption.”
The authors hope their work inspires other groups to conduct similarly collaborative research on diseases like FASD that benefit from drawing together medical and computational fields.
Source:
AIP
Media Contacts:
AIP Media Line – AIP
Image Source:
The image is credited to Gao Lin and Linda Sommerlade.
Original Research: Open access
“Quantitative assessment of cerebral connectivity deficiency and cognitive impairment in children with prenatal alcohol exposure”. Lin Gao, Celso Grebogi, Ying-Cheng Lai, Julia Stephen, Tongsheng Zhang, Yuanli Li, Hai Peng Ren, Dichen Li, Jue Wang, Bjoern Schelter and Linda Sommerlade.. Chaos. doi:10.1063/1.5089527
Abstract
Quantitative assessment of cerebral connectivity deficiency and cognitive impairment in children with prenatal alcohol exposure
It is common knowledge that alcohol consumption during pregnancy would cause cognitive impairment in children. However, recent works suggested that the risk of drinking during pregnancy may have been exaggerated. It is critical to determine whether and up to which amount the consumption of alcohol will affect the cognitive development of children. We evaluate time-varying functional connectivity using magnetoencephalogram data from somatosensory evoked response experiments for 19 teenage subjects with prenatal alcohol exposure and 21 healthy control teenage subjects using a new time-varying connectivity approach, combining renormalised partial directed coherence with state space modeling. Children exposed to alcohol prenatally are at risk of developing a Fetal Alcohol Spectrum Disorder (FASD) characterized by cerebral connectivity deficiency and impaired cognitive abilities. Through a comparative study of teenage subjects exposed to alcohol prenatally with healthy control subjects, we establish that the inter-hemispheric connectivity is deficient for the former, which may lead to disruption in the cortical inter-hemispheric connectivity and deficits in higher-order cognitive functions as measured by an IQ test, for example. We provide quantitative evidence that the disruption is correlated with cognitive deficits. These findings could lead to a novel, highly sensitive biomarker for FASD and support a recommendation of no safe amount of alcohol consumption during pregnancy.
Fetal alcohol spectrum disorders (FASDs), characterised by impaired cognitive abilities, are a group of conditions that can occur in a person whose mother has consumed alcohol during pregnancy. Surveys from the United States have found that about 10% of pregnant women have consumed alcohol in the last month and 20% to 30% at some point during the course of the pregnancy. Although there is clear evidence that children exposed to alcohol prenatally are at risk of developing an FASD, some studies have argued that the risk of problems depends on the amount consumed, the frequency of consumption, or when during pregnancy the alcohol was consumed. Our study involving experimental data collected from teenage subjects, combined with mathematical modeling, shows that there is no safe amount or safe stages during pregnancy for alcohol consumption. We employ a new time-varying connectivity approach to estimate the fast changing information flow among the brain sources using magnetoencephalogram data of somatosensory evoked response experiments from 19 teenage subjects with prenatal alcohol exposure (PAE) and 21 healthy control (HC) teenage subjects. We demonstrate that the inter-hemispheric connectivity is deficient for subjects with prenatal alcohol exposure. A lack of the inter-hemispheric connectivity is known to facilitate autism, stroke, schizophrenia, as well as dementia, disrupts the cognitive performance, and may lead to neurobehavioral deficits. We show that the disruption in the inter-hemispheric connectivity observed in this study is correlated with cognitive deficits associated with FASD, suggesting a potential new biomarker for FASD. Based on our findings, we support the recommendation of no safe amount of alcohol during pregnancy.






